Acupuncture and herbal medicine show effectiveness in alleviating symptoms of Long COVID. Chronic COVID-19 (Long COVID) involves diverse conditions caused by acute COVID-19 that begin weeks, months, or years after the acute phase. Researchers tested the efficacy of Chinese herbal medicine combined with acupuncture for the treatment of this condition. The results show significant outcomes when using acupuncture and herbal medicine.
The Clinical Global Impression (CGI) scale of SF-36 scores before and after treatment were analyzed with SPSS 26.0 software. Significant improvement was defined as complete or substantial elimination of symptoms or signs. Effective treatment was marked progress in symptoms or signs or partial elimination of symptoms. The results show that among the 31 cases in the study, 23 cases (74.19%) were significantly effective after treatment, and 8 cases (25.81%) were effective. All patients showed improvements with no ineffective cases.
Common symptoms that were improved or eliminated were fatigue, chest tightness and shortness of breath, insomnia, dream disturbed sleep, headaches, palpitations, memory loss, and sweating. Additional symptoms that were improved or eliminated were back pain, coughing, low appetite, aversion to cold, dysosmia, anosmia, difficulty breathing, dizziness, dry mouth, thirst, soreness of the extremities, sore throat, hair loss, skin disorders, visual and auditory disorders, and gastrointestinal problems. The total effective rate was 100% with no adverse reactions. The study was marked by high compliance.
The Ping'an Hospital (Xicheng District, Beijing) research included 11 males and 20 females with Long COVID in the clinical trial. The following herbs were administered: modified Sheng Mai Yin combined with Yu Ping Feng San. The base formula included: Radix Salviae Miltiorrhizae (Danshen) 30g, Radix Astragali (Huangqi) 15g, and Radix Ginseng (Taizishen), Ophiopogon tuber (Maidong), Fructus Schisandrae (Wuweizi), Rhizoma Atractylodis Macrocephalae (Bai Zhu), and Radix Saposhnikoviae (Fangfeng) 10g each.
Herbs were added for specific symptom presentations. For cough and phlegm: Herba Ephedrae (Mahuang) and Ramulus Cinnamomi (Guizhi) 9g each, and Rhizoma Zingiberis (Gan Jiang) and Rhizoma Pinelliae (Ban Xia) 10g each. For wind-cold cough: Fructus Trichosanthis (Gualou) 20g, Pericarpium Citri Reticulatae (Chenpi), Bulbus Allii Macrostemonii (Xiaobai), and Radix Platycodi (Jiegeng) 10g each. For cough, sore throat, and constipation: Periostracum Cicadae (Chantui) and Bombyx Batryticatus (Jiangcan) 10g each, and Radix et Rhizoma Rhei (Dahuang) 9g.
For qi deficiency and blood stasis with chest pain, shortness of breath, back pain, and palpitations: Radix Salviae Miltiorrhizae (Danshen) 30g, Semen Persicae (Taoren) 24g, Rhizoma Chuanxiong (Chuanxiong), Cortex Cinnamomi (Rougui), Lignum Sappan (Sumu) 10g each, and Hirudo (Shuizhi) 3g. For phlegm and blood stasis with chest pain, shortness of breath, back pain, and excessive phlegm: Radix Salviae Miltiorrhizae (Danshen) 30g, Fructus Trichosanthis (Gualou), Bulbus Allii Macrostemonii (Xiaobai), and Rhizoma Pinelliae (Ban Xia) 10g each, and Hirudo (Shuizhi) 3g.
For qi stagnation and blood stasis with chest pain, shortness of breath, fatigue, and palpitations: Rhizoma Chuanxiong (Chuanxiong) and Semen Persicae (Taoren) 10g each, and Flos Carthami (Honghua) 3g. For qi and blood deficiency with fatigue, weakness, and hair loss: Radix Astragali (Huangqi) 50g and Radix Angelicae Sinensis (Danggui) 10g.
A water decoction of 400ml was orally ingested daily and divided into 2 doses, taken in the morning and evening. A total of 6 doses constituted 1 course of treatment, and 3 courses were applied.
Acupuncture was applied five days per week for three weeks, with 15 treatments completing the course of treatment. The following acupuncture points were applied with 0.25 mm x 25 mm needles:
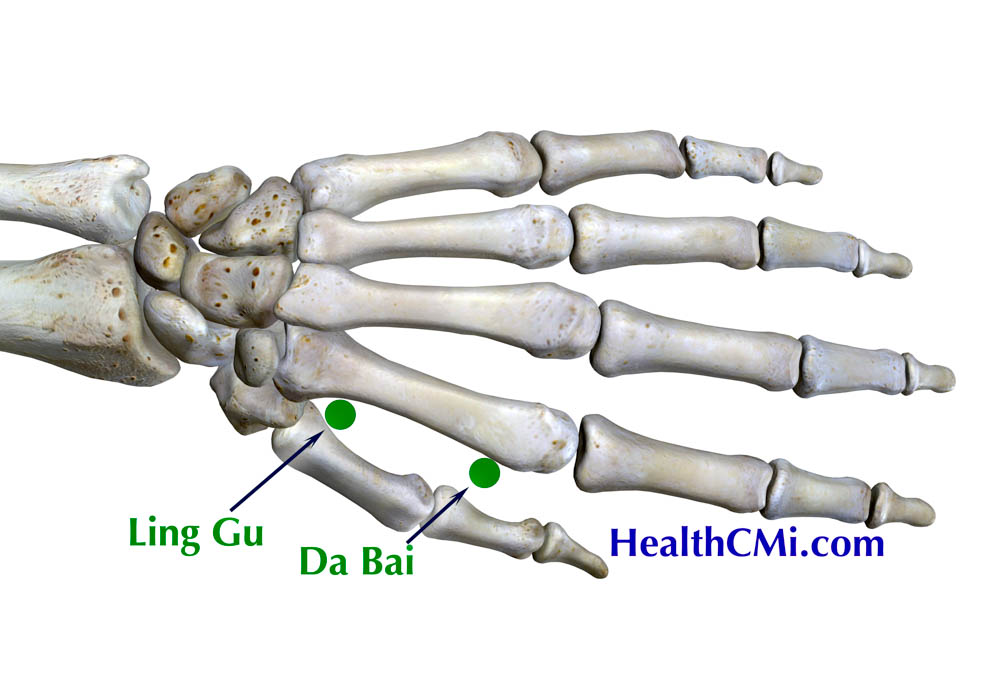
- Linggu (灵骨, Spirit Bone, 22.05)
- Dabai (大白, Great White, 22.04)
- LU9 (Taiyuan)
- LU10 (Yuji)
- LU7 (Lieque)
- GV20 (Baihui)
The following acupoints received 0.35 mm x 50 mm needles:
- GV14 (Dazhui)
- ST36 (Zusanli)
Moderate standard stimulation with even reinforcing and reducing techniques were applied and needles were retained for 40 minutes. After obtaining qi sensation, moxibustion was attached to the handle of GV14. Shield guards of aluminum foil for heat protection were used.
Linggu (灵骨, Spirit Bone, 22.05) and Dabai (大白, Great White, 22.04) acupoints belong to Master Tung's Dao Ma technique of unique acupuncture points. Linggu acupoint is located on the interosseous space between the thumb and index finger at the junction of the first and second metacarpal bones. Dabai acupoint is located on the back of the hand between the first and second metacarpal bone, approximately one inch distal from the Linggu acupoint. The results of this investigation indicate that acupuncture and herbal medicine are helpful in recovery from Long COVID.
Reference:
[1] Chen Huanjun, Yang Ruikang, and Xiao Cunli. "Clinical observation on the recovery period of new coronavirus infection treated with combined acupuncture and medicine." Shanxi Traditional Chinese Medicine 39.08(2023):43-45.


