Researchers have discovered that acupuncture is effective for controlling overactive bladder syndrome. The research team, a combination of Whipps Cross University Hospital and University College of London Hospital investigators, document that 79% of patients in the study showed clinically significant improvements. 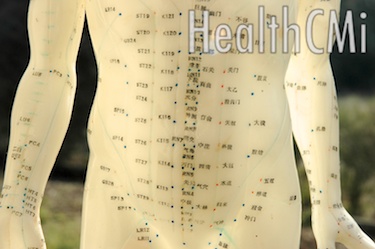 The researchers conclude that acupuncture is an effective treatment modality for patients with overactive bladder syndrome (OAB) and “is well tolerated with no side effects or complications.” As a result, the research team notes that acupuncture “should be considered as a potential alternative to our current therapeutic regimes” for patients with OAB.
The researchers conclude that acupuncture is an effective treatment modality for patients with overactive bladder syndrome (OAB) and “is well tolerated with no side effects or complications.” As a result, the research team notes that acupuncture “should be considered as a potential alternative to our current therapeutic regimes” for patients with OAB.
Overactive bladder syndrome is a dysfunction of the bladder’s storage abilities that lead to a sudden urge to urinate. Symptoms include a sudden urge to urinate that is often difficult to control, involuntary loss of urine (urge incontinence), frequent urination (greater than 8 times per day) and waking at night 2 or more times to urinate (nocturia). Etiology varies and may include dysfunction of the kidneys, bladder nerve signals and muscle activity. Contributing and exacerbating factors of OAB include multiple sclerosis (MS), Parkinson’s disease, increased fluid intake, kidney and bladder organic disorders, diabetes, pharmaceutical medications and illicit drugs, urinary infections, enlarged prostate and increased consumption of caffeinated beverages.
The researchers note that acupuncture is safe and effective. All patients in the study had already tried conventional approaches to care: behavioral modifications and pharmaceutical medications including anticholinergics and beta agonists. Although surgical procedures are often part of conventional treatment regimes of care for OAB sufferers, all candidates were pre-surgical. The research team notes, “The aim of the study is to assess if acupuncture is effective in the treatment of patients with OAB in whom conservative measures and oral medications have failed, but are unwilling or unsuitable for invasive therapies.”
This study focused on 3 acupuncture points. This protocolized approach is common in scientific investigations and varies from standard clinical practice in which customization of the acupuncture point prescription is applied for specific diagnostic considerations. Despite the limitations of a standardized set of acupuncture points across all patients in the study, 79% of all patients showed significant clinical improvements. In a real-life situation, a licensed acupuncturist has the ability to adjust the protocol to meet the specific individual needs of the patients. As a result, a licensed acupuncturist can potentially exceed the success rate achieved in this protocolized approach to care.

Acupuncture was applied at a rate of once per week for a total of 10 weeks. Each acupuncture treatment session was 30 minutes in length. Acupuncture points SP6, CV4 (RN4) and KI3 were applied. SP6 and KI3 were needled bilaterally on the lower leg and ankle. CV4 (RN4) was needled on the midline and is depicted in the image at top of the article. The researchers note that the study began with the use of traditional manual acupuncture and later electroacupuncture was applied to the needles. Urodynamic studies and evaluations confirm that this regime of care is both safe and effective for the treatment of overactive bladder syndrome.
The researchers note that acupuncture has several benefits. It can be used for patients who cannot tolerate medications, acupuncture does not cause the adverse effects associated with OAB medications, acupuncture demonstrated efficacy where medications and behavioral therapy failed and acupuncture may avert the need for surgery as a corrective measure. Acupuncture provides an effective option to patients who have tried medications without success. In this way, acupuncture can potentially reduce the number of patients requiring surgery for OAB.
References:
Post-treatment, Pre-treatment, and ICIQ-UI Short Form. "ACUPUNCTURE IN THE MANAGEMENT OF OVERACTIVE BLADDER SYNDROME." 2014.
Philp T, Shah PJR, Worth PHL. Acupuncture in the treatment of bladder instability. British Journal of Urology 1988 Jun: 61(6); 490-493.


