Acupuncture is found equally effective as taking a pharmaceutical medication for the treatment of overactive bladder. This condition is a dysfunction of urination bladder storage leading to sudden urges to urinate. In many cases, this may lead to the inability to control the loss of urine, incontinence. Symptoms include sudden urges to urinate, frequent urination, nocturia (frequent nightime urination) and urge incontinence (loss of urine caused by an urge to urinate). 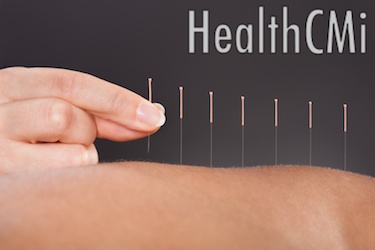
Researchers confirm that acupuncture is 90% effective in treating overactive bladder. The drug solifenacin, also known as Vesicare®, is 86.9% effective. Adverse effects that may be caused by the pharmaceutical medication include dry mouth, dry eyes, constipation, stomach pain, burning urination, extreme thirst, nausea, vomiting, painful urination, difficulty breathing, blurry vision and extreme exhaustion. Acupuncture does not involve the risk of these side effects and may therefore be preferable for some patients. Solifenacin is contraindicated for patients with pernicious glaucoma, myasthenia gravis, severe liver disease and for those undergoing kidney dialysis. The new research proves that acupuncture provides an effective treatment option for patients unable to take solifenacin.
The Investigation
The acupuncture continuing education study was conducted at the Department of Urology in the Second Affiliated Hospital of Guiyang College of Traditional Chinese Medicine. A total of 60 patients with overactive bladder (OAB) were randomly divided into two groups. Group #1 took solifenacin via oral administration. Group #2 received acupuncture treatments. After the completion of a four week long treatment regime, both groups achieved significant progress. Notably, acupuncture did not cause any side effects and was found both safe and effective.
Drug Dose
Patients in group #1 took 4 mg of solifenacin via oral administration once daily after breakfast. One course of treatment consisted of 4 weeks for both groups. Patients in both groups were forbidden from receiving any other treatments to eliminate variables from the investigation.
The Acupuncture Treatment
Group #2 received acupuncture with filiform needles that ranged between 1.5 - 4 cm in length and diameters ranging from 0.32 - 0.38 mm. During the procedure, patients rested in the prone or supine position. The acupuncture points applied were:
Guanyuan (CV 4)
Shenshu (BL 23)
Zuwuli (LR 10)
Yinlingquan (SP 9)
Shuidao (ST 28)
Zhongji (CV 3)
Zhonglvshu (BL 29)
Pangguangshu (BL 28)
Ciliao (BL 32)
Manual acupuncture manipulation techniques were applied to acupoints:
CV 4
BL 23
LR 10
SP 9
ST 28
Light stimulation and the heavy-thrusting-light-lifting reinforcing methods were used. Strong stimulation using the heavy-lifting-light-inserting reducing method was applied to:
BL 29
BL 28
CV 3
The retention of needling was 30 minutes and one minute of manual manipulation was applied every 10 minutes. The acupuncture treatment was applied once a day for four weeks. 
The Results
The researchers compared average frequency of urinary urgency, average frequency of urination, nocturnal enuresis, average urine volume and frequency of urinary incontinence between the two groups. The solifenacin group produced 4 patients cured, 23 patients having made remarkable progress and 4 patients having made no progress. The acupuncture group produced 5 patients cured, 22 patients having made remarkable progress and 3 patients having made no progress. The overall effective rate for the acupuncture group was 90% compared with 86.9% for the solifenacin group. Given the statistically similar effective rates, the researchers conclude that acupuncture is as effective as solifenacin in treating overactive bladder.
Reference:
Wang, Bo, Youping Xiao, Kai Fan, Congjun Huang. “Treatment of female overactive bladder with acupuncture.” Journal of Beijing University of Traditional Chinese Medicine 36.10 (2013): 713-716.


