Acupuncture reduces pain and improves functional mobility for patients with osteoarthritis. Researchers from the University of Manitoba, Canada, conducted a meta-analysis of 12 trials consisting of 1,763 patients with osteoarthritis. All trials compared true acupuncture with sham acupuncture, conventional treatments and no treatments.  The study finds acupuncture effective in reducing pain intensity levels, increasing mobility and improving quality of life scores. A subgroup analysis reveals that patients receiving acupuncture treatments for intervention periods greater than 4 weeks have greater reductions in pain intensity levels than patients receiving acupuncture over a shorter duration of time.
The study finds acupuncture effective in reducing pain intensity levels, increasing mobility and improving quality of life scores. A subgroup analysis reveals that patients receiving acupuncture treatments for intervention periods greater than 4 weeks have greater reductions in pain intensity levels than patients receiving acupuncture over a shorter duration of time.
Osteoarthritis is the most common form of arthritis and affects millions of people worldwide. It affects joints in the body including the hands, lower back, neck, knees and hips. This type of arthritis is often associated with ‘wear and tear’ degeneration of joint cartilage over time. Risk factors include aging, diabetes, injuries, gout, hypothyroid conditions and obesity. Symptoms and signs include pain, lack of flexibility and bone spurs.
Conventional treatments include medications to control pain and inflammation, physical therapy, occupational therapy, cortisone and hyaluronic acid derivative injections, and joint replacement surgery. The Mayo Clinic staff notes on their website that studies show acupuncture, Tai Chi and yoga may help reduce osteoarthritis pain and improve mobility. This University of Manitoba study confirms that acupuncture is effective in the treatment of osteoarthritis.
The researchers cite several modern investigations finding acupuncture effective for the treatment of several types of pain related conditions including fibromyalgia, lower back pain and osteoarthritis. Their investigation also cites studies demonstrating that acupuncture is a cost-effective treatment and is a “safe non-pharmacological treatment of musculoskeletal pain.” The researchers note, “we found acupuncture administered to adults with osteoarthritis to be associated with a statistically significant reduction in pain intensity, improved functional mobility and improved health-related quality of life.”
The researchers note that the most common acupuncture points used for the sample size of 1,763 patients were ST36, ST34, Xiyan, GB34, and SP9. Other acupuncture points include SP10, ST40, LV3, ST44, GB29, SP5, DU20, BL60, GB43, GB30, and extra points including EX31, EX32, and EXLE5. Most studies included manual acupuncture techniques to evoke de qi at least once during each treatment period. De qi is a combination of bodily sensations induced by acupuncture needling combined with physiological responses to the stimulation. De qi sensation is often described as dull, heavy, deep pressure, pulling, numb, aching, spreading, radiating, electrical, refreshing, relieving and tingling.
Huazhong University of Science and Technology researchers measured de qi’s relationship to changes in blood flow, tissue displacement, myoelectricity and brain MRI signals. They note “intrinsic change(s) of (the) human body” are induced by de qi during acupuncture. The team added that the “de qi elicited significant response(s) to acupuncture in (the) specific brain regions….” Other researchers note that achieving de qi at acupuncture points elicits distinctly different cortical responses than at non-acupuncture points. Specific acupuncture points demonstrate a consistent and unique ability to stimulate specific brain regions upon de qi stimulation. By contrast, non-acupuncture points did not induce unique responses. Researchers from the Beijing University of Chinese Medicine, Medimar International Hospital and the European Foundation of TCM performed a meta-analysis of the medical implications of de qi. The findings suggest a direct correlation between ancient acupuncture techniques and improved positive patient outcomes. 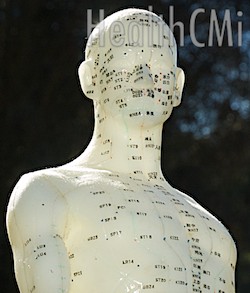
The osteoarthritis researchers at the University of Manitoba note studies showing that, “Electrical needle stimulation can enhance the effects of acupuncture.” This study only examined manual acupuncture and excluded electro-acupuncture to eliminate electrical stimulation as a variable. The sorting process was stringent and excluded non-randomized studies and studies wherein superficial needling was used as part of the sham acupuncture techniques. The researchers found 14,449 relevant citations and sifted this number down to 12 unique trials of 1,763 patients to ensure that only quality studies were examined in the meta-analysis.
Several important strengths become apparent. First, manual acupuncture without any additional electrical stimulation is effective in the treatment of osteoarthritis. Acupuncture was found both safe and effective in the quality studies reviewed. Additionally, acupuncture was found cost-effective for the treatment of osteoarthritis.
The findings are not unique. For example, research published in Rheumatology, one of the Oxford Journals, concludes that “Sham-controlled RCTs suggest specific effects of acupuncture for pain control in patients with peripheral joint OA (osteoarthritis). Considering its favourable safety profile acupuncture seems an option worthy of consideration particularly for knee OA.” That study examined 18 randomized controlled trials of both manual and electro-acupuncture. The wide body of research supporting the use of acupuncture for the treatment of osteoarthritis as a safe and cost-effective modality suggests that further integration into biomedical settings and protocols is warranted.
References:
Manyanga, Taru. "Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis." BMC Complementary and Alternative Medicine 2014, 14:312.
Tian, Dai-Shi, Jin Xiong, Qing Pan, Fang Liu, Lu Wang, Sha-Bei Xu, Guang-Ying Huang, and Wei Wang. "De Qi, a Threshold of the Stimulus Intensity, Elicits the Specific Response of Acupoints and Intrinsic Change of Human Brain to Acupuncture." Evidence-Based Complementary and Alternative Medicine 2014 (2014).
Zhu, Shi-Peng, Li Luo, Ling Zhang, Song-Xi Shen, Xiao-Xuan Ren, Meng-Wei Guo, Jia-Min Yang et al. "Acupuncture DE-qi: from Characterization to Underlying Mechanism."
Chen, Sheng, Shengnan Guo, Federico Marmori, Yanping Wang, Qi Zhao, Baokai Wang, Eunhae Ha et al. "Appraisal of the De qi Concept among Contemporary Chinese Acupuncturists."
Kwon, Y. D., M. H. Pittler, and E. Ernst. "Acupuncture for peripheral joint osteoarthritis A systematic review and meta-analysis." Rheumatology 45, no. 11 (2006): 1331-1337.


