Researchers find acupuncture more effective than an SSRI antidepressant medication for the treatment of post-stroke depression and prove that acupuncture combined with Chinese herbs are effective for stroke rehabilitation.
Researchers from Zhejiang Chinese Medical University and Hainan Provincial People’s Hospital finds acupuncture and traditional Chinese herbal medications effective in alleviating post-stroke conditions. The Xing Shen Jie Yu acupuncture method is effective in treating post-stroke depression; administering the herbal decoction Bu Yang Huan Wu Tang with acupuncture combats stroke sequelae. In both investigations, acupuncture treatment delivered significant positive patient outcomes.

Acupuncture is effective in treating post-stroke depression. Researchers from Zhejiang Chinese Medical University determined that a particular method of acupuncture, Xing Shen Jie Yu, which employs electroacupuncture, is more effective than standard medications in treating post-stroke depression. Post-stroke Depression (PSD) is a mental disorder that may present in post-stroke patients. Compared with patients without PSD, the depression that plagues PSD afflicted patients inhibits the speed of neurological rehabilitation after the stroke occurs. Consequently, PSD patients find it harder to regain a satisfactory level of independence and quality of life. Research has shown that the rate of PSD occurrence falls between 20 – 50% (Gaete and Bogousslavsky, 2008).
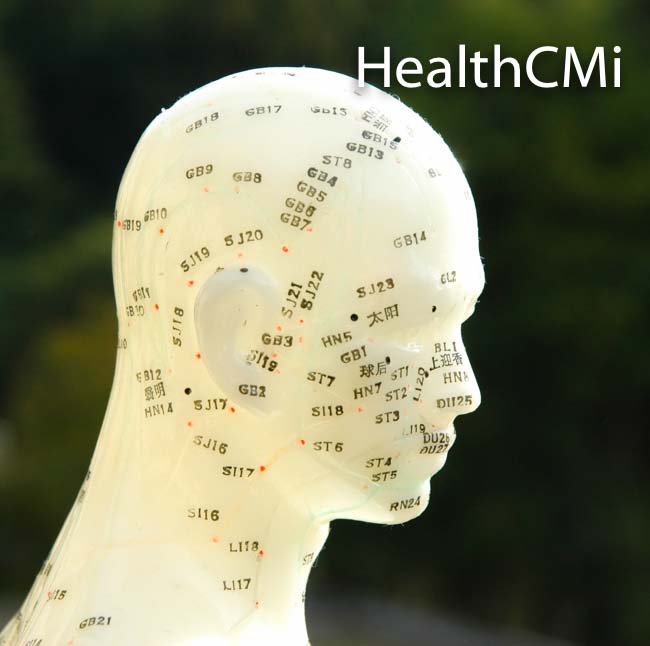
Xing Shen Jie Yu acupuncture is a characteristic method of acupuncture that was established by China’s renowned Traditional Chinese Medicine (TCM) doctor, Professor Wang Zhang Lian. The primary acupoints in Xing Shen Jie Yu are: Baihui, Shenting, Sishencong, Zusanli, Sanyinjiao and Taichong. The electroacupuncture technique utilized in Xing Shen Jie Yu significantly increases nerve and cerebral cortex stimulation, and produces a higher concentration of 5-HT and NE in brain tissue and cerebrospinal fluid.
The acupuncture classic Zhen Jiu Da Cheng (Great Compendium on Acupuncture and Moxibustion) dictates that the Governor meridian should be targeted in the treatment of brain illnesses; the Baihui and Shenting acupoints are both located along this meridian. Administering acupuncture on these acupoints can improve qi and blood circulation along the Governor meridian, reinforce the Yang element, and fight depression. It is worth noting that the Baihui, Shenting and Sishencong acupoints are located on the frontal lobe surface projection zone. Therefore, acupuncture administration on these acupoints increases neuronal excitability as well as neurotransmitter secretion. The Zusanli acupoint also regulates qi and blood circulation in addition to dredging the meridians. The Taichong acupoint has a tranquilizing effect. The Sanyinjiao acupoint is a major acupoint for maintaining and improving spleen, liver and kidney health.
In the study conducted by researchers at Zhejiang Chinese Medical University, patients who received Xing Shen Jie Yu acupuncture reported a 93.33% total treatment effective rate, whereas those in the control group reported a 90% rate. The Xing Shen Jie Yu acupuncture group also displayed better performance in daily living activities performance. This research studied 60 PSD patients who were divided into two groups, the treatment group and the control group. The treatment group underwent Xing Shen Jie Yu acupuncture and the control group received citalopram medication. Citalopram is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. Both groups received standard post-stroke treatments including blood pressure, blood glucose, and blood lipid regulation, as well as rehabilitation.
The acupoints used for the treatment group include the primary acupoints in Xing Shen Jie Yu acupuncture:
- Baihui (GV20)
- Shenting (GV24)
- Sishencong (EX)
- Zusanli (ST36)
- Sanyinjiao (SP6)
- Taichong (LV3)
Additional acupoints were selected on a symptomatic basis. For facial paralysis, the following acupoints were chosen:
- Jiache (ST6)
- Dicang (ST4)
- Yinxiang (LI20)
For speech impairment, the following acupoints were chosen:
- Lianquan (CV23)
- Tongli (HT5)
For upper limb paralysis, the following acupoints were chosen:
- Jianyu (LI15)
- Quchi (LI11)
- Shousanli (LI10)
- Waiguan (TH5)
- Hegu (LI4)
- Houxi (SI3)
For lower limb paralysis, the following acupoints were chosen:
- Huantiao (GB30)
- Futu (ST32)
- Yanglingquan (GB34)
- Yinlingquan (SP9)
- Xuanzhong (GB39)
- Jiexi (ST41)
A 0.25 mm X 40 mm disposable acupuncture needle was used for each acupoint. A different technique of insertion was applied for each acupoint, as described:
For the Baihui acupoint, the needle was inserted transversely and posteriorly between a depth of 0.5 – 0.8 inches, thereafter manipulating it with a rotating (Nian Zhuan) technique at a speed of 200 rotations/minute, for a total of 2 minutes. For the Sishencong acupoints, the needle was inserted transversely and towards the Baihui acupoint, between a depth of 0.5 – 0.8 inches. The front Sishencong acupoint was paired with the left Sishencong acupoint, and the back Sishencong acupoint with the right Sishencong acupoint. Both pairs of acupoints were then connected to Han’s Acupoint Nerve Stimulator with 100 Hz frequency. After the area surrounding the acupoints displayed visible pulsing, and patient comfort was optimal, the Han’s Acupoint Nerve Stimulator was used to apply electroacupuncture stimulation for 30 minutes. For the Shenting acupoint, the needle was inserted transversely and anteriorly between a depth of 0.5 – 0.8 inches, thereafter manipulating it with a rotating (Nian Zhuan) and reinforcing (Bu) technique at a speed of 200 rotations/minute, for a total of 2 minutes. For the Zusanli acupoint, the acupuncture needle was inserted perpendicular-obliquely, towards the direction of the tibia, between a depth of 1 – 2 inches, with the reinforcing (Bu) technique. For all acupoints, the needle retention time was 30 minutes. An acupuncture session was conducted once daily, 6 times per week, with a 1 day break between weekly sessions. A full treatment course comprised 30 days of acupuncture sessions.
For the control group, patients took one 20 mg citalopram tablet per day, after breakfast. A full medication course comprised 30 continuous days. The treatment effective rate for all patients in the study was evaluated based on the Hamilton Depression Scale rating, and categorized as follows:
- Recovery: Rating reduction of at least 75%.
- Significantly effective: Rating reduction of at least 50%.
- Effective: Rating reduction of at least 25%.
- Ineffective: Rating reduction of less than 25%.
Both the treatment and control groups showed positive patient outcomes. However, the Xing Shen Jie Yu acupuncture group had a 93.33% total treatment effective rate, whereas the citalopram medication group had a 90% total treatment effective rate. Based on the clinical results of the study, Xing Shen Jie Yu acupuncture produces more positive patient outcomes than citalopram medication in treating post-stroke depression. Given the effectiveness of both types of patient care, a study on the effectiveness of combining acupuncture and citalopram therapy is warranted.
Another study reflects equally important positive patient outcomes regarding the effectiveness of Traditional Chinese Medicine modalities in treating stroke related conditions. Researchers from Hainan Provincial People’s Hospital determined that acupuncture and the decoction Bu Yang Huan Wu Tang have a synergistic efficacy in treating stroke sequelae. Traditional Chinese Medicine supplements acupuncture to increase the total treatment effective rate. Strokes are a common occurrence. Stroke patients are frequently plagued with disabilities and risk of fatality and relapse. Stroke sequelae refers to hemiplegia, aphasia or other disorders which persist after more than half a year following the occurrence of stroke. As such, research into the effectiveness of treatment modalities for post-stroke syndrome is of great import.
The herbs used in Bu Yang Huan Wu Tang have been proven by modern pharmacologic research to be beneficial for the body in various ways. Astragalus is an effective antioxidant and improves bodily microcirculation. By virtue of this, it can increase the superoxide dismutase activity in the brain and improve brain resistance against hypoxia (Shen, 1995). Radix paeoniae rubra, semen persicae, angelica and rhizome of Szechuan lovage are all herbs that improve blood circulation, eliminate blood stasis, and reduce capillary permeability and intracranial pressure, thereby alleviating cerebral hematomas.
The Qihai acupoint promotes qi circulation and reinforces the yang. The Zusanli acupoint significantly reduces excesses of plasma fibrinogen. The Guanyuan acupoint stimulates blood cell restoration and improves blood supply to the brain. The combined effect of these acupoints is to revitalize the cerebral cortex, amplify nerve regulatory function, and expedite body cell and tissue metabolism — essentially healing the central nervous system.
In the study conducted by researchers at Hainan Provincial People’s Hospital, stroke sequelae patients who received treatment with acupuncture and Bu Yang Huan Wu Tang achieved a 90.63% total treatment effective rate, whereas those in the control group reported a lower total treatment effective rate of 75%.
This research included 60 patients receiving therapy for stroke sequelae. The patients were divided into two groups: the treatment group and the control group. The treatment group underwent acupuncture treatment and were given the Bu Yang Huan Wu Tang decoction. The control group received salvia fluid intravenous infusion. Both groups received conventional neurological treatment, which included the use of: mannitol to reduce intracranial pressure, nimodipine to regulate blood pressure, and citicoline sodium to revitalize brain cells.
The primary acupoints selected for the treatment group can be categorized by location. The acupoints located on the upper limbs include:
- Jianguo
- Quchi (LI11)
- Shousanli (LI10)
- Neiguan (PC6)
- Hegu (LI4)
The primary acupoints located on the lower limbs include:
- Huantiao (GB30)
- Weizhong (UB40)
- Zusanli (ST36)
- Yanglingquan (GB34)
- Xuehai (SP10)
- Chengshan (UB57)
- Sanyinjiao (SP6)
- Taixi (KD3)
- Taichong (LV3)
The primary acupoints located on the face and head include:
- Baihui (GV20)
- Fengfu (GV16)
- Taiyang (EX)
- Dicang (ST4)
- Zanzhu (BL2)
- Renzhong (GV26)
- Xiaguan (ST7)
- Yamen (GV15)
- Lianquan (CV23)
For each acupuncture session, 8 – 10 acupoints were selected for each of the 3 aforementioned treatment areas. Upon the arrival of deqi sensation, a needle retention time of 30 minutes was observed. Each acupuncture session was conducted once daily. The standard ingredients for the Bu Yang Huan Wu Tang decoction are as follows:
- Astragalus, Huang Qi (60 – 80g)
- Angelica, Dang Gui (20g)
- Red peony root, Chi Shao (20g)
- Earthworm, Di Long (20g)
- Rhizome of Szechuan lovage, Chuan Xiong (20g)
- Semen persicae, Tao Ren (10g)
- Safflower, Hong Hua (10g)
Additional herbs were added on a symptomatic basis:
- Cooked and prepared common monkshood daughter root (Fu Zi) , for excess of the chill element
- Codonopsis (Dang Shen) and atractylodes (Bai Zhu), for weak spleen and stomach
- Concretio silicea banbusae (Tian Zhu Huang) and pinellia (Ban Xia), for excessive phlegm
- Hemp seed (Ma Zi Ren) and seed of Chinese bushcherry (Yu Li Ren), for constipation
The decoction was prepared once daily, taken over two doses per day, once in the morning and once at night. For the control group, 30ml of salvia (Dan Shen) fluid was administered via intravenous infusion.
Administering acupuncture and Bu Yang Huang Wu Tang achieved a higher total treatment effective rate of 90.63% over that of administering salvia fluid through intravenous infusion, which achieved 75%. Based on the clinical results of the Hainan Provincial People’s Hospital study, acupuncture and Bu Yang Huan Wu Tang combine effectively to heal stroke sequelae.
The above studies are a clear indication of the success of acupuncture in producing positive patient outcomes in stroke patients. With these scientifically validated results, acupuncture should be considered more often as a treatment option for patients recovering from stroke. Moreover, the introduction of acupuncture and herbal medicine into conventional medical settings introduces potential for increasing positive patient outcomes across a large population.
References:
Hong ZM, Wang ZL, Zhang SQ & Ma RJ. (2015). Observation on Effect of "Xing Shen Jie Yu" Acupuncture Method in Treating post-stroke Depression. Journal of Zhejiang Chinese Medical University. 39(8).
Gaete JM, Bogousslavsky J. Post-stroke depression[J] .Expert Rev Neurother, 2008(8): 75-92.
Zhou SJ. (2012). Buyang Huangwu Decoction and Acupuncture Treat Stroke Sequelae 60 cases. Journal of Zhejiang Chinese Medical University. 36(6).
Shen YJ. (1995). Traditional Chinese Medicine Pharmacology. Shanghai: Shanghai Technology Publisher. 164-165.


