Acupuncture and acupoint herbal plaster therapy increase positive patient outcomes for patients with chronic coughing.
In a controlled investigation, acupuncture outperformed drug therapy for the treatment of chronic coughing following the acute stage of a respiratory infection. Another investigation finds acupoint herbal plaster therapy effective for improving patient outcomes for children with chronic coughing. In an integrative approach to patient care, acupoint herbal plaster therapy enhanced patient outcomes for children receiving standard drug therapy.
 Location of ST36 (Zusanli)
Location of ST36 (Zusanli)
An investigation by Li and Shi finds acupuncture more effective for the treatment of chronic coughing than drug therapy. Li and Shi conducted their controlled trial in Tangshan (China). They tested the efficacy of acupuncture versus methoxyphenamine, a bronchodilator that is a β-sympathomimetic agent. The acupuncture points tested were limited to the Lung-Taiyin and Stomach-Yangming acupuncture channels. The results tabulated, acupuncture produced significantly greater patient outcomes. As a result, researchers conclude that acupuncture is more effective for the treatment of post-infectious chronic coughing than methoxyphenamine. Acupuncture produced a 90% total treatment effective rate and drug therapy produced an 80% total treatment effective rate.
The clinical trial investigated chronic coughing in humans that was initially caused by an acute phase of a respiratory infection. Chronic symptoms include dry coughing, throat irritation, scanty white phlegm or no phlegm, etc. Biomedical treatments include antitussive, antihistamine, decongestant, and antibiotic medications. According to Traditional Chinese Medicine (TCM) theory, a persistent post-infectious cough is in the scope of Wan Ke (persistent cough) or Jiu Ke (prolonged cough).
Chronic coughing TCM treatment principles often focus on expelling wind and dredging the lungs, dependent upon differential diagnostic pattern differentiations. While expelling the wind sounds archaic or unscientific to the western mind, it is simply another lexicon describing specific biophysical events. As an example, the sweating (Han Fa) technique is one of the expel wind modalities. According to TCM, using diaphoretic acupuncture techniques or herbal medicines expels wind to release pathogenic influences. Expelling wind is semantically external to conventional biomedical terminology yet refers to biomedically definable processes. The principles of expelling wind are correlated with specific, quantifiable biomedical phenomena. The same holds true for dredging the lungs, which often refers to clearing toxins and phlegm from the respiratory system.
Li and Shi chose a protocolized set of acupuncture points for the research based on Lung-Taiyin and Stomach-Yangming channel principles. They note that, in TCM, acupuncture on these channels benefits the lung and stomach organs. Citing the research of Duan, Zhou, and Gao, they add that lung-stomach theory postulates Ju Yu Wei, Guan Yu Fei (accumulation in the stomach gathers in the lungs).
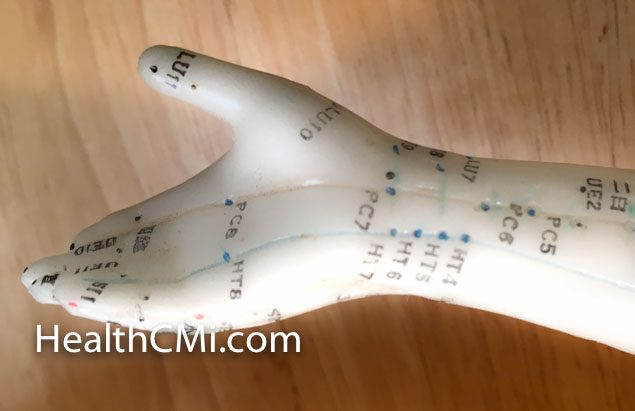
Three treatment groups were compared. Ninety patients were randomly divided into the three groups. Treatment group 1 received acupuncture on both Lung-Taiyin and Stomach-Yang channel acupoints. Treatment group 2 received acupuncture on Lung-Taiyin acupoints and treatment group 3 received drug therapy (methoxyphenamine capsules). The group treated with Lung-Taiyin and Stomach-Yang channel acupoints had a 90% total effective rate. Using only Lung-Taiyin acupoints yielded an 83.3% total effective rate. Drug therapy produced an 80% total effective rate. The primary acupoints selected for treatment group 1 were the following:
- Yuji (LU10)
- Chize (LU5)
- Kongzui (LU6)
- Lieque (LU7)
- Tianshu (ST25)
- Zusanli (ST36)
- Fenglong (ST40)
After standard disinfection, a 0.30 mm X 40 mm filiform needle was inserted into each acupoint, and the Ping Bu Ping Xie manipulation technique was applied. Upon arrival of a deqi response, the needle was left in position for a needle retention time of 30 minutes. One 30 minute acupuncture session was conducted per day. The entire course of treatment comprised 10 sessions. The primary acupoints selected for treatment group 2 were the following:
- Yuji (LU10)
- Xiabai (LU4)
- Zhongfu (LU1)
- Chize (LU5)
- Kongzui (LU6)
- Lieque (LU7)
The Zhongfu, Chize, Kongzui, Taiyuan and Yuji acupoints are located along the lung meridian. According to TCM principles, administering acupuncture to these acupoints improves qi and blood circulation, heals coughing and asthma, and improves lung health (Xu, 2007). Signature acupoints needled along the stomach meridian are Tianshu, Zusanli, and Fenglong. The acupuncture protocol for treatment group 2 was identical to treatment group 1. One 30 minute acupuncture session was conducted per day. The entire course of treatment comprised 10 sessions. Methoxyphenamine capsules for treatment group 3 were taken orally, 3 times per day, 2 capsules each time, for 10 consecutive days.
Patients’ cough symptoms were scored before and after treatment according to the Cough Diagnosis and Treatment Guidelines of 2009. A score of 0 – 3 was given to patients based on the severity of cough symptoms. The treatment effective rate after the full treatment course was calculated based on changes in the score before and after treatments. Treatment efficacy for each patient was categorized into 4 tiers:
- Recovery: No cough symptoms. Treatment effective rate ≥95%.
- Significantly effective: Very few cough symptoms. Treatment effective rate between 70% – 90%.
- Effective: Significant improvement in symptoms. Treatment effective rate between 30% – 69%.
- Ineffective: No improvement in symptoms. Treatment effective rate ≤30%.
Based on the clinical data of Li and Shi’s study, acupuncture based on the lung-stomach theory produces excellent patient outcomes in the treatment of post-infectious coughing. Also, acupuncture outperformed drug therapy. Based on TCM principles, the researchers note that the lung-stomach theory does not target coughing as an isolated symptom, but rather promotes overall bodily health to achieve clinical efficacy.
In another related study, researchers Chen et al. from Chancheng Central Hospital (Foshan, China) find Yongquan and Feishu acupoints useful in treating pediatric coughing in conjunction with standard drug therapy. In this research, Chen et al. explored the efficacy of applying the Yuan Hong Wai antitussive plaster to both Yongquan and Feishu. They found that acupuncture on both acupoints produced better patient outcomes than only on Feishu. The pediatric coughing examined in this study is a common disease equivalent to bronchitis. According to TCM principles, infantile coughing arises due to impacted lung functioning, either by external pernicious influences or internal organ dysfunction.
Yuan Hong Wai antitussive plasters are an experimental treatment method in TCM that displays varying treatment efficacies when applied on different acupoints. The antitussive plaster treatment method combines the medicinal effects of TCM, acupoints, and meridians. Its focus is to stimulate acupoints and improves qi and blood circulation. Upon external application, the TCM medicinal components in the plaster are absorbed through the skin and subsequently delivered to afflicted body tissues, effectively treating diseases by restoring normal organ function. The action of this treatment method is classified under the “external treatment of internal disease” TCM treatment concept.
Two additional studies have also investigated Yuan Hong Wai antitussive plasters and their effect on coughing in children. Zhang applied plasters on the Yongquan acupoint combined with an acupoint injection. Yu et al. applied plasters on the Yongquan acupoint as well. Both studies achieved significant positive patient outcomes. In the Chen et al. study, patients receiving the Yuan Hong Wai plater on Feishu and Yongquan reported a total treatment effective rate of 92%. Patients receiving the Yuan Hong Wai plaster on only Feishu reported a total treatment effective rate of 81%.
The Yuan Hong Wai plaster study involved a sample size of 400 cough patients, ages 1 – 7 years. They were randomly divided into two equal groups: two acupoint treatment group, single acupoint treatment group. Both groups received antibiotics and other standard medications for coughing, phlegm, and asthma. Both groups then received application the Yuan Hong Wai antitussive plaster on the following acupoints. For the two acupoint group:
- Feishu (BL13)
- Yongquan (KD1)
For the single acupoint group:
- Feishu (BL13)
Both groups followed the same treatment protocol. For each acupoint, the area around the acupoint was cleaned using a warm and damp towel. Next, the protective film on the plaster was removed. The plaster was then adhered to the acupoint firmly. If required, an additional medicinal plaster was used to affix and secure the plaster. A new plaster was freshly applied once per day, for 4 – 6 hours each time, for 3 consecutive days. The combined protocol of drug therapy with the plaster therapy is part of an integrative medicine approach to care. The researchers investigated the plasters to determine additional non-invasive treatment modalities that improve patient outcomes for children receiving standard care. Treatment efficacy was categorized into 3 tiers:
- Recovery: No cough. No sign of dry or phlegmy wheezing upon stethoscopy.
- Improvement: Cough mitigated. Clear breathing sound. Decrease in phlegm.
- Ineffective: No improvement in cough, or symptoms worsened.
Chen at al. conclude that the double acupoint application is superior to the single acupoint application of the plaster. As a result, Chen at al. formally recommend the double acupoint protocol. Additionally, Chen at al. recommend more research into other possible acupoints that may increase the positive patient outcomes for children receiving the herbal plaster therapy.
The aforementioned studies indicate that acupuncture and acupoint plaster therapy are effective. Plaster therapy enhances standard care outcomes. Acupuncture outperformed drug therapy. Overall, the investigators find that Traditional Chinese Medicine approaches to patient care benefit patients with chronic coughing related conditions.
References:
Li XQ & Shi ZM. (2015). Acupuncture Treatment Based on Lung-stomach Theory in Treating Post-infectious Cough. Shanghai Journal of Acupuncture and Moxibustion. 34(3).
Duan YP, Zhou J & Gao LJ (2003). Analysis on lung-stomach theory. Shanxi Journal of TCM. 24(12):1104-1106.
Xu ZH. (2007). Warm moxibustion combined with acupoint external application in treating post-fever cough: 26 cases. Journal of Clinical Acupuncture. 23(9): 45-50.
Chen QZ, Chen JX, Deng XX. Clinical Observation on Treatment with Application at Yongquan Acupuncture Point and Feishu Acupuncture Point for 200 cases of Infantile Cough.
Chinese Journal of Ethnomedicine and Ethnopharmacy.
Yu MF, Zeng RX, Lei XG, et al. (2008). TCM External Application on Yongquan Acupoint in Treating Infantile Cough. Journal of External Therapy of Traditional Chinese Medicine. 17(5): 8-10.
Zhang WL. (2000). Yongquan Acupoint External Application and Acupoint Injection in Treating Infantile Cough: 35 Cases. Shanghai Journal of Acupuncture. 19(1): 42.


