Electroacupuncture halts accidental urinary leakage and restores bladder control.
Researchers demonstrate that electroacupuncture is safe and highly effective for the treatment of urinary incontinence in women. Electroacupuncture significantly reduced urgency and leakage. Electroacupuncture restored long-term bladder control and produced a 78.6% total effective rate.
Acupuncture is effective for the treatment of urinary incontinence in women. China Academy of Chinese Medical Science researchers (Jin et al.) conclude that electroacupuncture produces significant positive patient outcomes for women with mixed urinary incontinence (MUI). Electroacupuncture produced a total effective rate of 78.6%. All metrics demonstrated significant clinical improvements: International Consultation on Incontinence Questionnaire – Short Form (ICI-Q-SF), 3-day urinary diary, 24-hour urine collection test. The overall ICI-Q-SF total score of 16 prior to electroacupuncture improved to 8 after treatments. The mean occurrence of urinary incontinence over 24 hours was reduced by 66.67% after treatments with electroacupuncture. The mean quantity of urinary leakage over 24 hours was 39 g before treatments and 18.6 g after treatments with electroacupuncture.
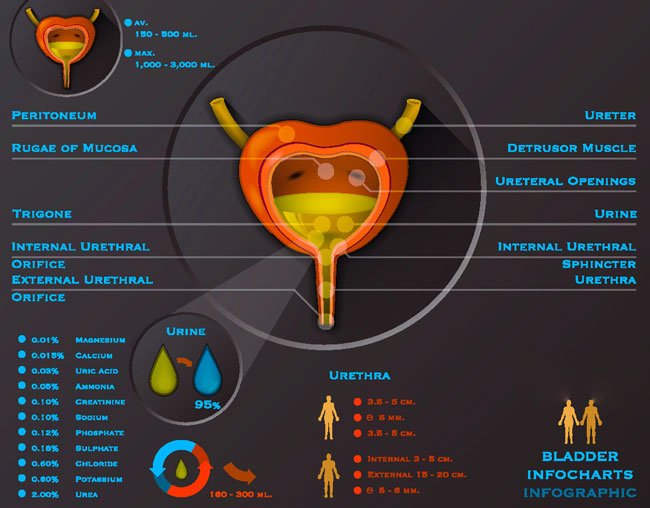
Mixed urinary incontinence (MUI) involves involuntary leakage of urine when sneezing, coughing, during exertion, and leakage associated with urgency. MUI accounts for approximately 30% of all women suffering from incontinence. The USA National Institutes of Health (NIH) notes that MUI is the primary form of incontinence. MUI has the characteristics of stress urinary incontinence (SUI) and urge urinary incontinence (UUI). Detrusor hyperactivity may also be involved in MUI. The detrusor muscle forms a layer in the wall of the urinary bladder.
MUI is on the rise in China. Currently, the rate of occurrence stands at approximately 9.4%. Tension-free vaginal taping of the obturator muscles is applied in standard care settings, with limited treatment results; the long-term total treatment effective rate is 30% (Jain et al.) for taping. The obturator muscles cover the exterior and anterior aspect of the pelvis bilaterally and are active in thigh and hip movements.
The researchers began their acupuncture investigation based on prior research demonstrating the efficacy of electroacupuncture for the treatment of MUI. Neurologic investigations in the field of urology demonstrate that specific acupuncture points have specific effective actions. The Ciliao (BL32) acupoint regulates the activity of sacral micturition center capsaicin receptor VR1, P substance concentrations in the spinal dorsal horn, calcitonin related peptides, and the activity of afferent C fibers. Regulation of these processes produces clinical results by mitigating MUI symptoms.
The Huiyang (BL35) acupoint regulates functioning of the detrusor muscles and the urethral sphincter. Performing electroacupuncture on both Ciliao and Huiyang strengthens pelvic support tissues by increasing the concentration of type I and type III collagen. The Sanyinjiao acupoint regulates detrusor and urethral sphincter coordination and regulates abdominal leak-point pressure. Additionally, acupuncture on the Zusanli (ST36) acupoint has been found to significantly regulate the binding force of muscarinic receptors in the cerebral cortex and spinal cord.
A total of 42 female patients diagnosed with MUI participated in this research. Subjects were aged between 41 – 72 years, with a mean age of 58 years. All subjects received a confirmed diagnosis of MUI based on clinical symptoms, 3-day urinary frequency, and the 24-hour urinary leakage test. Participants were also cleared of the possibility of urinary tract infection, bladder outlet obstruction, and pelvic outlet prolapse. All patients underwent electroacupuncture therapy. The primary acupoints selected were:
- Ciliao (BL32)
- Huiyang (BL35)
- Shenshu (BL23)
- Zusanli (ST36)
- Sanyinjiao (SP6)
Treatment commenced with the patient in a supine or prone position. After disinfection with 75% alcohol, a 40 mm x 0.3 mm disposable acupuncture needle was inserted into each acupoint, following standard insertion depths. Upon arrival of a deqi sensation, the needle was left in position. Next, the Ciliao and Huiyang acupoints were connected to the positive and negative electrodes of the electroacupuncture device. A disperse-dense wave was used for 30 minutes, with an initial dense wave frequency of 4 Hz and an initial disperse wave frequency of 20 Hz. The intensity was gradually increased according to patient tolerance levels. One 30 minute acupuncture session was conducted 3 times a week, for a total of 8 weeks. Treatment efficacy was measured by calculating pre-treatment and post-treatment scores for these aspects:
- Clinical symptoms: based on the ICI-Q-SF
- Urinary incontinence frequency: based on the 3-day urinary diary
- Urinary leakage: based on the 24-hour urine collection test
Treatment efficacy was then categorized into 3 tiers:
- Recovery: No urinary incontinence, or 24-hour urinary leakage <2 g.
- Effective: ICI-Q-SF total score reduced by ≥50%, or 24-hour urinary leakage reduced by ≥50%.
- Not effective: No significant improvement in symptoms, or 24-hour urinary leakage reduced by ≤50%.
The total treatment effective rate was calculated as the percentage of patients who achieved at least the effective treatment tier. Based on the results, the researchers conclude that electroacupuncture is an effective procedure for the treatment of urinary incontinence. Moreover, medications and surgical procedures were not used or needed for the procedure or production of positive patient outcomes. The researchers note that the procedure is safe, easily applied by an acupuncturist, and is relatively non-invasive compared with surgical interventions used in standard care settings. Given the high degree of safety and efficacy, electroacupuncture is recommended for the treatment of MUI.
Given that this research covers the importance of electroacupuncture, the following is a summary of one electroacupuncture device’s abilities. At the Healthcare Medicine Institute, we have not received any funding to include the following information by the manufacturer of the electroacupuncture device or any other source. The information is solely intended for informational purposes only and is an effort to highlight tools of the acupuncturist.
Tools of the Trade
Electroacupuncture involves the application of specialized electro-stimulators to acupuncture needles. One unit is the ITO ES-160 Physiotherapy & Rehabilitation device. This electroacupuncture device features standard frequency and intensity controls to six channels. Each channel has a positive and negative electrode connector for a grand total of twelve needles that can be connected to the device.
The unit is known for its ability to adjust the width of the pulse in microseconds. It includes a customizable timer and programmable memory system for a variety of treatment combinations. Standards settings include constant, burst, surge, fast-slow (disperse-dense), sweep, and three additional programmed sequences.
The high and low frequencies are adjustable on disperse-dense and sweep modes. There is even an optional audible feedback system to monitor the pulse of the waves. Perhaps the most important aspect of the unit is its compact design, clear layout, and easily operated controls with built-in safety features. The device includes six electrodes and a search-stimulator probe with grounding unit. This unit includes the sweep mode, which is not available on many other electroacupuncture units. Unlike a standard disperse-dense wave, which alternates between two frequencies, the sweep mode gradually shifts from the slower frequency setting to the faster setting followed by a gradual slowing to the original slower frequency before repeating the cycle.
References:
Jin CL, Zhou XY & Pang R. (2013). Effect of electro-acupuncture on mixed urinary incontinence in women. Journal of Clinical Acupuncture and Moxibustion. 29(6).
Jain P, Jirschele K, Bostros SM, et al. (2011). Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 22(8): 923-932.


