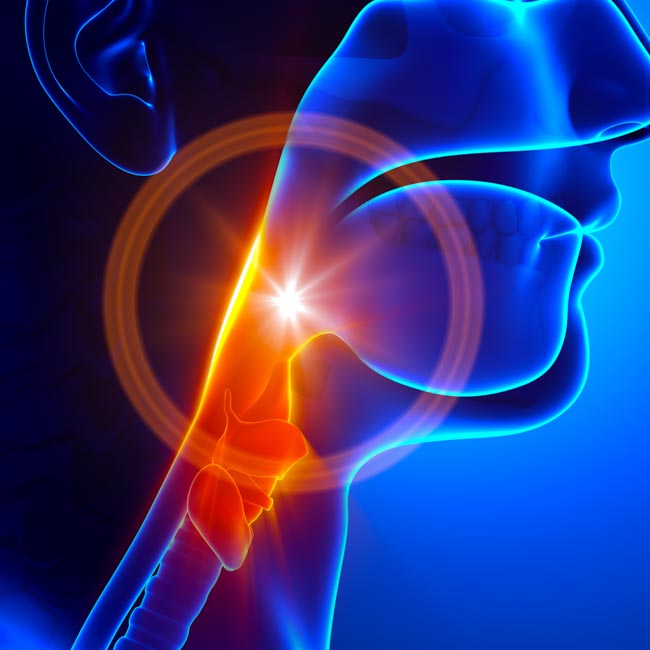
Acupuncture is an effective treatment modality for the restoration of swallowing after a craniocerebral injury (CCI). Brain injuries may result in dysphagia, a disorder involving difficulty or discomfort when swallowing. Researchers conducted a randomized controlled trial and determined that acupuncture combined with neuromuscular electrical stimulation and rehabilitation exercises is an effective treatment protocol for the treatment of dysphagia after a CCI.
Wang et al. studied 90 patients with dysphagia caused by craniocerebral injuries. This included patients with several pathologies including traumatic brain injuries, cerebral infarctions, and cerebral hemorrhages. The participants were randomized into three groups. Group A was provided conventional rehabilitation exercises. Group B was given rehabilitation exercises plus neuromuscular electrical stimulation. Group C was given rehabilitation exercises, neuromuscular electrical stimulation, and acupuncture.
All patients were treated over the course of 4 weeks, and their swallowing abilities, degree of swallowing difficulties, and daily quality of living before and after the treatments were compared. The group having received acupuncture as part of a comprehensive recovery program had the highest improvements across several measures: VFSS, WST, SWAL-QOL.
The VFSS (Videofluoroscopic Swallowing Study) is a barium swallowing examination employing real-time x-rays for the visualization of bolus flow and structural movements in the aerodigestive tract. The VFSS is particularly helpful in determining improvements for swallowing food and developing strategies toward restoring oral nutrient intake. Patients receiving acupuncture had the greatest improvements as confirmed by the VFSS.
The WST (water-swallowing test) is a functional exam that detects aspiration and is useful in developing strategies to prevent pneumonia. The WST assesses drinking and its relation to successful swallows, swallowing speed, time to swallow, coughing, choking, or otherwise having to stop ingestion of water. As with the VFSS, the group receiving acupuncture had the greatest improvements in the WST.
The SWAL-QOL (Swallowing Quality of Life Questionnaire) evaluates 44 items and 10 quality of life components to determine patient satisfaction and the quality of therapeutic care. Again, the group receiving acupuncture had the greatest improvements in the SWAL-QOL. The results were published in a study entitled Clinical Observation on Neuromuscular Electrical Stimulation Combined with Acupuncture and Rehabilitation Exercise for Relieving Dysphagia in Patients with Craniocerebral Injury by Wang et al.
A total of 90 dysphagia patients with craniocerebral injuries participated in the clinical trial. There were 53 males and 37 females with an average age of 58 and an average medical history of 4.6 weeks. A total of 43 patients were cases with cerebral infarction, 24 cases with cerebral hemorrhage, 13 cases with traumatic injury, and 10 other cases of CCI. They were randomly split into 3 groups: A, B and C.
All patients were greater than 18 years of age and VFSS confirmed swallowing difficulties prior to inclusion in the study. All patients signed consent letters and were approved by an ethics committee. Exclusion criteria included patients with esophagus or neck tumors, mental impairment, disorders of consciousness, mental illness, damage in lung function, connective tissue disease, and disorders of homeostasis.
The research team detailed their clinical protocols for the investigation. All groups received rehabilitation exercises and treatments to address nourishment, protection of brain cells, reduction of skull pressure, and prevention of dehydration. Group A received only these treatments and no other forms of care. The rehabilitation exercises included the following:
- cold stimulation
- practicing of swallowing
- breath hold techniques
- voicing exercises
- throat contraction exercises
- throat lifting exercises
- face and lips muscle functional training
Rehabilitation exercises were conducted once daily, 30 minutes each time, for a total of four weeks of continuous treatments. Group B received additional care. Neuromuscular electrical stimulation was administered. The electrode was connected to the handheld electrode stimulator (battery powered) and placed at the neck. This was administered once per day, 30 minutes each time, for a total of four weeks.
Group C received the aforementioned treatments plus acupuncture. The needle retention period was 30 minutes each session and the needles were manipulated every 15 minutes. Acupuncture treatments were administered once per day, for a total of 30 minutes each session, for 4 continuous weeks. The following lists the acupuncture protocol and acupoints administered to the patients:
Xiaguan ST7 (Below the Joint)
Use of 1.5 inch acupuncture needles to a depth of 1 inch with mild pulling, pushing, and twisting techniques to elicit deqi was administered.
Jiache ST6 (Jaw Bone)
Use of 1 inch acupuncture needles to a depth of 0.5 inches deep with twisting techniques to elicit deqi was applied.
Dicang ST4 (Earth Granary)
Use of 1 inch acupuncture needles to a depth of 0.5 inches deep with twisting techniques to elicit deqi was applied.
Tongli HT5 (Penetrating the Interior)
Use of 1 inch acupuncture needles inserted perpendicularly to depth of 0.8–1 inch deep with pulling, pushing, and twisting techniques to elicit deqi was applied.
Hegu LI4 (Joining Valley)
Use of 1 inch acupuncture needles inserted perpendicularly to depth of 0.8–1 inch deep with pulling, pushing, and twisting techniques to elicit deqi was applied.
The researchers cite Traditional Chinese Medicine (TCM) principles as the basis for the acupoint selections. TCM notes that dysphagia is caused by meridian blockages affecting the tongue and throat. Blockages are due to wind, phlegm, qi, and blood stasis. Acupuncture meridians innervating the throat and tongue are of principle concern; these include the shaoyin, taiyin, yangming, taiyang, du, ren, and shaoyang meridians. Acupoints were chosen based on activation of the channels.
The results of the study demonstrate that acupuncture is an effective tool in a comprehensive approach to dysphagia related patient care. Objective and subjective measures of improvement demarcate specific clinical gains made by the addition of acupuncture to a therapeutic protocol. The quality of life and health of patients is contingent upon surmounting difficulties and complications associated with dysphagia. This includes prevention of pneumonia, the ability to receive adequate nutrition orally, and avoidance of both choking and coughing. Based on the evidence, implementation of acupuncture into inpatient and outpatient therapies is recommended.
References
Wang, H. M., Cai, C. & Zhang, Z. F. (2015). Clinical Observation on Neuromuscular Electrical Stimulation Combined with Acupuncture and Rehabilitation Exercise for Relieving Dysphagia in Patients with Craniocerebral Injury. Journal of Nanjing University of Traditional Chinese Medicine. 31 (2).
Wang, S. X., Wang, Q., An, X. L., et al. (2013). Effect of swallowing function training and acupuncture and neuromuscular electrical stimulation on dysphagia after cerebral apoplexy [J]. Hebei Med J. 35 (20): 3175-3176.


