Researchers conclude that acupuncture increases the clinical effective rate of the drug cefodizime for the treatment of acute exacerbations of chronic cholecystitis (inflammation of the gallbladder). Xining Haihu Hospital researchers combined acupuncture with standard drug therapy. Patients receiving both drug therapy and acupuncture in a combined treatment protocol had superior patient outcomes compared with patients using only drug therapy. The drug control group achieved a total effective rate of 50.0%. The acupuncture plus drug treatment group achieved a total effective rate of 98.0%. The addition of acupuncture to the administration of cefodizime increases the total effective rate by 48%.
The VAS (Visual Analogue Scale) scores in the acupuncture plus drugs group were significantly better. The addition of acupuncture to drug therapy also produced significant improvements in the value of serum bilirubin and biochemical markers of liver functions. The researchers conclude that the combination of acupuncture plus drug therapy is safe and effective for the treatment of chronic cholecystitis. Let’s take a closer look at the results.
The study design was as follows. A total of 100 patients were randomly distributed into a control group and a treatment group, each consisting of 50 cases. The control group received drug therapy. The treatment group received acupuncture plus the same drug therapy administered to the control group. All patients were diagnosed with chronic cholecystitis between May 2015 and May 2016.
The statistical breakdown for each randomized group was as follows. The acupuncture treatment group was comprised of 30 males and 20 females. The youngest patient in the acupuncture treatment group was 38 years of age, the oldest was 58 years. The average age was 51 (±1) years. The average height in the acupuncture treatment group was 163.7 (±1.4) cm. The drug control group was comprised of 35 males and 15 females. The youngest patient in the drug control group was 39 years of age, the oldest was 57 years. The average age was 51 (±1) years. The average height in the drug control group was 165.2 (±1.3) cm. There were no significant statistical differences in terms of gender, age, and height relevant to patient outcome measures prior to beginning the investigation. Inclusion criteria were as follows. All participants were diagnosed with chronic cholecystitis. They met the following inclusion criteria:
- Right upper abdominal pain, radiating to the right shoulder
- A prolonged course of disease, with repeated attacks of acute cholecystitis
- Tenderness or percussion pain in the gallbladder region, may be accompanied by a positive Murphy’s sign
- A rough, thickened gallbladder wall seen on ultrasound and CT, may be accompanied by gallstones
Exclusion criteria were applied. Patients who had the following conditions did not participate in the study:
- Comorbid gallbladder perforation, generalized peritonitis, acute obstructive suppurative cholangitis, and acute gangrenous cholecystitis
- Prone to bleeding
- Unable to follow instructions from researchers due to ambiguous consciousness or psychosis
- Pregnant or lactating
The control group and the acupuncture treatment group received identical medications. A total of 1 g of cefodizime for intravenous injections was administered once daily, for a total of 7 consecutive days. Cefodizime is a broad spectrum cephalosporin antibiotic, commonly used in clinical treatments. In addition, the treatment group received acupuncture. The acupoints for acupuncture therapy were as follows:
- GB34 (Yanglingquan)
- Dannangxue (Extra M-LE-23)
- LV3 (Taichong)
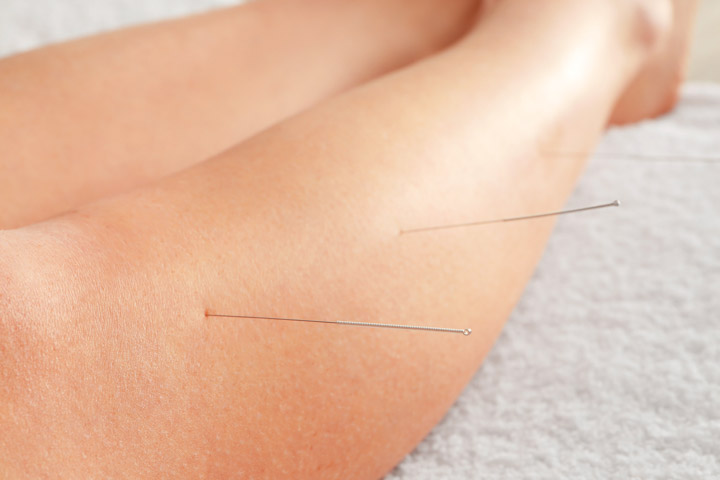
Treatment commenced with patients in a supine position. After disinfection of the acupoint sites, a 0.30 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed, until a deqi sensation arrived. For Taichong, the rotating technique was applied up to three times, until involuntary twitching of the leg muscles was observed. For Yanglingquan, the needle was perpendicularly inserted to a depth of 25—30 mm and manipulated with mild reinforcing and attenuating (Ping Bu Ping Xie) techniques. For Dannangxue, the needle was perpendicularly inserted to a depth of 20 mm and manipulated with mild reinforcing and attenuating techniques. Following the manual acupuncture stimulation procedures, a needle retention time of 50 minutes was observed per acupuncture session. The acupuncture sessions were conducted once daily for 7 consecutive days. After treatment completion, the treatment efficacy for each patient was categorized into 1 of 3 tiers:
- Recovery: Normal serum bilirubin levels. Normal results for liver function tests.
- Effective: Total bilirubin decreased by 17–25.5 μmol/L. Significant improvement in results for liver function tests.
- Not effective: No improvement in total bilirubin values and results for liver function tests.
Patients were evaluated before and after the treatment course. Both subjective and objective instruments were used to measure patient outcomes. All patients underwent Visual Analogue Scale (VAS) assessment before and after their treatments. VAS is a measurement instrument that measures pain intensity levels experienced by patients. Next, serum bilirubin values, including total bilirubin (TBIL) and direct bilirubin (DBIL), and biochemical markers of liver functioning, such as ALP and GGT, were measured.
It is important to note that chronic cholecystitis falls under the Xietong (Rib-side Pain) class of disorders in Traditional Chinese Medicine (TCM). Chronic cholecystitis is characterized by right upper abdominal pain. Exacerbations include pain becoming severe after exhaustion or an emotional upset. Biliary colic occurs when there is an acute exacerbation of chronic cholecystitis with a gallstone lodging in the cystic duct. Its symptoms include abdominal pain in the right upper quadrant or epigastric region, and pain occasionally radiating to the right shoulder, back, or lower back. In addition, nausea, vomiting, and fever can be present.
According to TCM principles, Taichong is a Yuan point as well as a Shu point (Bei Shu) on the foot jueyin liver meridian. Needling this point benefits the liver and gallbladder by abating dampness and jaundice. Yanglingquan is a He-Sea point on the foot shaoyang gallbladder meridian. Needling Yanglingquan increases gallbladder smooth muscle contractility and biliary secretion. In addition, Yanglingquan provides a pain relieving effect for patients suffering from cholecystitis by relieving spasms of the sphincter of Oddi.
The extra point Dannangxue (translated as gallbladder point) is traditionally indicated for the treatment of cholecystitis, cholelithiasis, gallstones, and biliary colic. Zhou et al. verify that needling Dannangxue normalizes the contraction of the common bile duct, increases peristalsis in the common bile duct, and thus reduces pain caused by cholecystitis. In addition, Wang et al. document that needling Dannangxue acts on the autonomic nervous system and provides a tranquilizing effect. It is valuable both as a diagnostic tool and a treatment acupoint. Palpation of Dannangxue is used to detect cholecystitis or cholelithiasis. Tenderness at the acupoint site is an indicator of gallbladder inflammation.
The research demonstrates that acupuncture is an effective adjunct treatment for the alleviation of gallbladder inflammation. Subjective and objective data supports the conclusions of the researchers in the controlled clinical trial. Based on the data, acupuncture increases the effectiveness of cefodizime for the treatment of gallbladder inflammation.
References
1. Yang ZY et al. Clinical Study of the Analgesic Effect of Acupuncture plus Medication on Acute Exacerbation of Chronic Cholecystitis [J]. Shanghai Journal of Acupuncture and Moxibution, 2017(3):291—294.
2. Wang SJ, Zhu B, Ren XX, et al. Experimental Study on Acupuncture Activating the Gonadotropin-releasing Hormone Neurons in Hypothalamus[J]. J Traditional Chinese Medicine, 2010, 30(1):30—39.


