Researchers find acupuncture combined with moxibustion effective for the alleviation of diabetic oculomotor paralysis. Xinjiang Medical University hospital researchers tested the efficacy of combining acupuncture and moxibustion with drug therapy. The addition of the Traditional Chinese Medicine (TCM) therapies increased positive patient outcomes by 45% for patients with diabetic oculomotor paralysis.
The researchers tested a protocol of drug therapy in combination with acupuncture and moxibustion in a controlled clinical trial. Drug therapy, as a standalone treatment, produced a 45% total effective rate. Adding acupuncture and moxibustion to the treatment regimen increased the total effective rate to 90%. Let’s take a look at the results.
The study design was as follows. The study involved the selection of 40 patients who received acupuncture and drug treatment at the Acupuncture and Neurology department of the First Affiliated Hospital of Xinjiang Medical University. Patients were randomly assigned to a TCM treatment group and a control group, with 20 patients in each group. Both groups received identical drug therapy. The treatment group was also treated with acupuncture and moxibustion.
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 13 males and 7 females, with an average age of 65 (±5) years and a disease course of 6.83 (±3.46) days. A total of 11 patients were affected on the left eye and 9 patients were affected on the right eye; 17 patients were affected on the oculomotor nerve and 3 patients were affected on the abducens nerve. The control group was comprised of 16 males and 4 females, with an average age of 65 (±7) years and a disease course of 7.42 (±2.63) days. A total of 13 patients were affected on the left eye and 7 patients were affected on the right eye; 12 patients were affected on the oculomotor nerve and 8 patients were affected on the abducens nerve. The patients from both groups were comparable as there were no significant differences in terms of their gender, age, disease course, and other factors of the disease.
Inclusion criteria were as follows. All participants were diagnosed with oculomotor paralysis according to the Standards for Diagnosis and Curative Effect of Chinese Medical Symptom system. In addition, patients participating in the study met the following inclusion criteria:
- A past medical history of diabetes
- Course of disease less than 15 days
- All genders, between 40—80 years of age
Exclusion criteria were applied. This assured that patients participating in the study suffered from diabetic oculomotor paralysis and not oculomotor paralysis secondary to other etiologies. Patients who had the following conditions did not participate in the study:
- Oculomotor paralysis due to intracranial tumors, intracranial aneurysm, myasthenia gravis, multiple sclerosis, infection, and trauma
- Course of disease lasting more than 15 days
- Age less than 40 years or more than 80 years
- Allergic to Vitamin B1 or having allergic constitution
- Prone to infection and bleeding or taking anticoagulant drugs
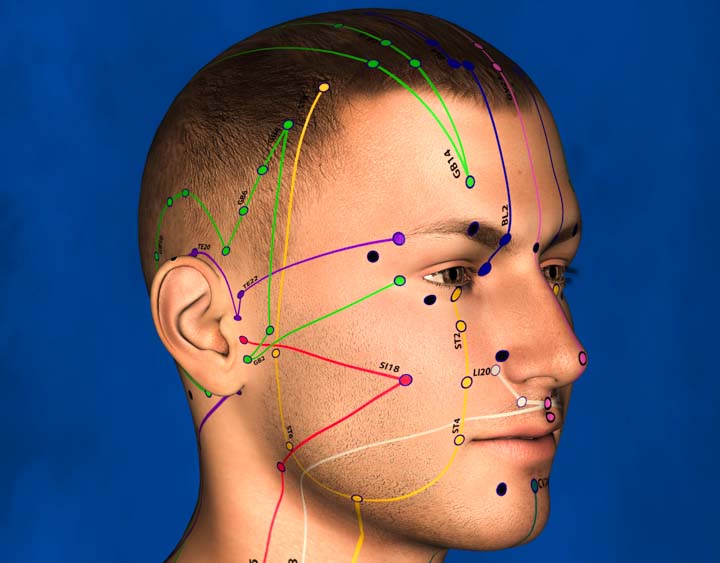
The treatment group received acupuncture, moxibustion, and drug therapy. The control group received only drug therapy. Both groups received identical medications. Patients from both groups consumed 400 mg of oral inosine tablets, 2 times per day, as well as 2 tablets of adenosine disodium triphosphate, 3 times per day. Inosine and adenosine disodium triphosphate were used to support the nervous system. In addition, the patients received 500 μg of mecobalamin (B12) injection, once per day. Mecobalamin is a cobalamin and used to treat diabetic neuropathy. All treatments lasted for 10 consecutive days. Next, patients from both groups switched to another drug therapy. They consumed 1 tablet of Vitamin B1, 3 times per day, as well as 1 tablet of mecobalamine, 3 times per day. Vitamin B1 and mecobalamine were used for nourishing the nerves. In addition, the patients received 0.5 g of Xueshuantong injection, once per day. Xueshuantong is an herbal medication used to promote blood circulation and remove blood stasis. It is comprised of Panax notoginseng (San Qi), Radix Astragali (Huang Qi), Radix Salvia Miltiorrhizae (Dan Shen), and Radix Scrophulariaceae (Sheng Di Huang). All treatments lasted for 14 consecutive days. In total, all patients received 24 days of medication treatment. The treatment group also received acupuncture and moxibustion. The acupoints selected for acupuncture therapy were as follows:
- GB14 (Yangbai)
- TB23 (Sizhukong)
- ST36 (Zusanli)
- SP6 (Sanyinjiao)
- KI3 (Taixi)
- LV3 (Taichong)
- ST2 (Sibai)
- LI4 (Hegu)
- ST7 (Xiaguan)
- TB17 (Yifeng)
- Shiqu (Extra)
- Yuyao (Extra)
- Taiyang (Extra)
Treatment commenced with patients in a supine position. After disinfection of the acupoint sites, a 0.30 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. The Wenbu (warming and reinforcing) manipulation technique was applied. A needle retention time of 30 minutes was observed. During needle retention, the needles were each manipulated with the same technique every 10 minutes. Next, moxibustion was applied to the following acupoints:
- ST7 (Xiaguan)
- ST36 (Zusanli)
Each acupoint was perpendicularly pierced with a 0.30 mm x 40 mm filiform acupuncture needle. Once a deqi sensation was obtained, the needles were retained and moxibustion was applied to the same acupoints. Moxa cigar cuttings, each 2 cm long, were attached to each needle handle and ignited. Moxa was left in place to self-extinguish. One session was conducted daily. Each treatment course consisted of 15 acupuncture and moxibustion treatments. All patients received 3 treatment courses in total. After treatment, the treatment efficacy for each patient was categorized into 1 of 3 tiers:
- Recovery: Complete alleviation of eye deviation. Movement of eyes regained completely. Absence of diplopia. No ptosis.
- Effective: Alleviation of eye deviation. Movement of eyes regained. Improvement of diplopia. Eyelid elevation more than 1 mm.
- Not effective: No alleviation of eye deviation, eye movement restriction, and diplopia. Eyelid elevation less than 1 mm.
The acupuncture treatment group had a total treatment efficacy rate of 90.0%. The medication control group obtained a 45.0% total treatment effective rate. The results demonstrate that acupuncture combined with moxibustion yields significant positive patient outcomes for patients with diabetic oculomotor paralysis.
Reference
Niu XL et al. Observations on the Efficacy of Warming-reinforcing Acupuncture plus Medication for Diabetic Oculomotor Paralysis [J]. Shanghai Journal of Acupuncture and Moxibustion, 2016, 35(11):1293—1295.


