Investigators find acupuncture effective for the treatment of IBS (irritable bowel syndrome). In a controlled study, Yiwu Central Hospital researchers conclude that acupuncture has a 90.7% total effective rate for IBS-D patients. Perhaps more importantly, acupuncture produces a 34.9% complete recovery rate. The total recovery rate accounts for all patients showing significant improvements and the complete recovery rate is a quantitative measure of all patients cured of IBS-D by acupuncture therapy.
Results were determined from both subjective and objective data. Subjectives were based on improvements in bowel movement frequency, shape, texture, and consistency. Subjectives also included measures of abdominal discomfort, anxiety, and sleep improvements. Objective data was based on changes of 5-hydroxytryptamine (5-HT), neuropeptide Y (NPY) and calcitonin gene-related peptide (CGRP) serum expression using automated ELISA analysers. The 90.7% total effective rate and the 34.9% complete recovery rate were calculated based on the the subjective and objective data.
About IBS
In this article, we are going to take a close look at the acupuncture points that achieved the results. First, let’s review a little about IBS before getting into the details. Irritable bowel syndrome (IBS) is a disorder affecting the digestive system. It is characterized by recurring abdominal pain and discomfort associated with alterations in the frequency of bowel movements or consistency of stool. At present, the occurrence of IBS is related to the patient’s history of gastroenterological viral infections, psychological factors, age, gender, occupation, history of medications, intestinal microflora balance, metabolic disorders of brain-intestinal axis, and other factors.
Based on the main pathological manifestations, IBS can be classified into four subtypes: IBS-D (diarrhea-predominant), IBS-C (constipation-predominant), IBS-M (mixed), and unspecified IBS (IBS-U). According to Traditional Chinese Medicine (TCM) principles, diarrhea-predominant IBS (IBS-D) belongs to the "diarrhea" (xie xie) and "abdominal pain" (fu tong) categories. The main causes of IBS are stagnation of liver qi, deficiency of the spleen and kidneys, and the invasion of cold and heat pernicious influences. [1] These result in gastrointestinal imbalances. TCM principles note that IBS is easily exacerbated by changes in the diet.
Design
Yiwu Central Hospital researchers conducted a two-arm study of 86 IBS-D patients between January 2016 and December 2016. [2] Patients were randomly divided into control group and an observation group, with 43 cases in each group. Patients were identified using the Rome III Diagnostic Criteria for Irritable Bowel Syndrome (IBS) as well as the TCM standards related to liver qi-stagnation and spleen-deficiency (gān yù pí xū) in the “Consensus on the Diagnosis and Treatment of Irritable Bowel Syndrome.” [3–4]
Patients in the control group were given the following herbal medicines over a 30-day period. The first medication was Spleen and Bowel-Reinforcing Pills (bǔ pí yì cháng wán), manufactured by China Resources Pharmaceutical Group Ltd. It was administered in 6-gram doses that were orally administered 3 times per day, after meals. In addition, patients were given herbal medicine in the form of Xiao Yao Wan (Hubei Wushi Pharmaceuticals) in 6-gram doses. The herbal pills were orally administered twice per day, after breakfast and after dinner.
Acupuncture Treatment
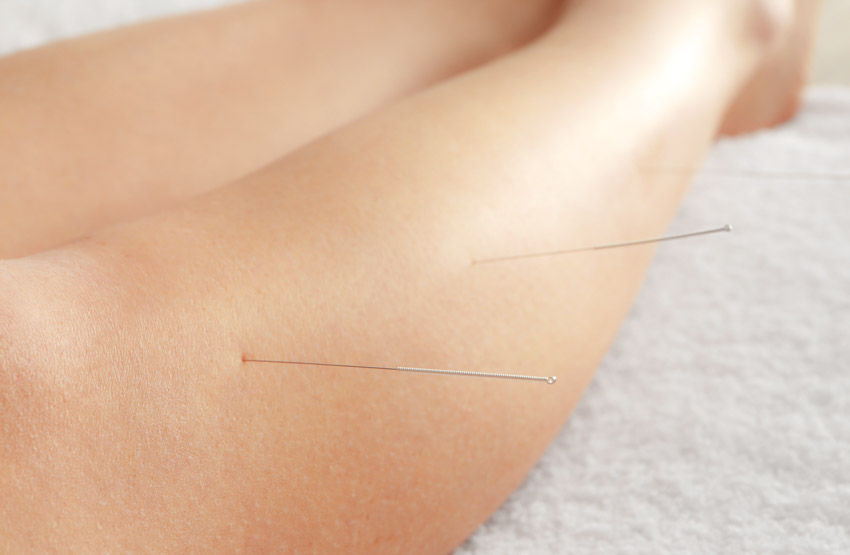
Patients in the observation group received acupuncture therapy in addition to the same herbal medicines administered to the control group. With patients in the supine position, needles were inserted swiftly to a depth of 20 mm. Twisting and reinforcing-reducing techniques were applied to achieve a deqi sensation of soreness, distention, numbness, or a radiating sensation towards the abdomen. Needles were then left in place for 30 minutes. The following are the acupoints used for all observation group patients:
- Yintang MHN3 (Hall of Impression)
- Baihui GV20 (Hundred Meetings)
- Shangjuxu ST37 (Upper Great Void)
- Tianshu ST25 (Heaven’s Pivot)
- Sanyinjiao SP6 (Three Yin Intersection)
- Zusanli ST36 (Leg Three Miles)
- Taichong LV3 (Great Rushing)
Twenty minutes of moxibustion therapy was also applied to the following acupoints:
- Shenque CV8 (Spirit Gateway)
- Tianshu ST25 (Heaven’s Pivot)
Patients experiencing severe diarrhea and cold syndromes received ginger moxibustion (ge jiang jiu) at Shenque CV8. Treatment was administered 5 times per week, over the course of 30 days.
Chinese Medicine
The above acupoints are key for benefitting the liver and spleen. The combined use of these acupoints is able to sooth the liver and strengthen the spleen (shu gan jian pi), firm the intestines and stop diarrhea (gu chang zhi xie), and promote the harmonious rise and fall of spleen and stomach qi. As IBS sufferers are prone to emotional disorders, acupuncture therapy at Yintang (MHN3) and Baihui (GV20) was added for a tranquilizing effect.
Efficacy of Treatment
Clinical efficacy was evaluated and compared after one course of treatment by assessing indicators such as main symptoms, psychological status, and sleep quality. Expressions of 5-hydroxytryptamine (5-HT), neuropeptide Y (NPY) and calcitonin gene-related peptide (CGRP) in serum samples were measured and compared before and after the intervention.
Main symptoms were scored based on the “Guiding Principles of Clinical Research on New TCM Drugs,” with each symptom given a score between 0 and 3. [5] The main symptoms included the following:
- Abdominal discomfort (0: no discomfort, 1: mild discomfort, 2: moderate pain, 3: severe pain)
- Stool frequency (0: 1 to 2 times/day, 1: 2 to 5 times/day, 2: 5 to 10 times/day, 3: ≥ 10 times/day)
- Shape, texture and consistency of stool (0: normal, 1: soft stool, 2: mushy stool, 3: watery stool)
- Presence of mucus in the stool and feeling of incomplete relief after bowel movement (0: never, 1: rarely, 2: frequently, 3: every time)
Psychological status of the patients was assessed using the Self-Rating Anxiety Scale (SAS) and the Self-Rating Depression Scale (SDS):
- SAS: Patients who scored 50–59 points had mild levels of anxiety, 60–69 points had moderate levels of anxiety, and ≥70 points had extreme levels of anxiety.
- SDS: Patients who scored 53–62 points had mild levels of depression, 63–72 points had moderate levels of depression, and >72 points had extreme levels of depression.
Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI), and was scored on a range of 0 to 21 points, with higher scores depicting better sleep quality. Serum levels of 5-HT, NPY, and CGRP were analyzed (5 mL of fasting peripheral venous blood was obtained from each patient 1 day before the start of treatment and one day after the entire course of treatment). Blood samples were centrifuged at 3000 r/min for five minutes to obtain the serum for analysis.
Efficacy standards were based on earlier research conducted by Affiliated Hospital of Shandong University of Traditional Chinese Medicine: [6]
- Treatment cured IBS: Absence of abdominal discomfort and related symptoms. Bowel movement appears normal and patients pass stool no more than 2 times daily.
- Treatment was highly effective: Significant improvement of various symptoms and reduction in stool frequency. Shape, texture and consistency of stool appear normal.
- Treatment was fairly effective: Alleviation of abdominal discomfort, reduction in stool frequency and improvement in shape, texture and consistency of stool.
- Treatment was ineffective: No improvement or worsening of the main symptoms.
Results
The recovery rate was 34.9% and the total effective rate was 90.7% in the observation group, versus 18.6% and 79.1% in the control group, and the total clinical efficacy of the observation group was significantly better than that of the control group (P<0.05). Both groups displayed significant improvements in the main symptoms after the intervention (P<0.05), with main symptoms scores of the observation group significantly better than those of the control group (P<0.05).
Both groups’ SAS, SDS, and PSQI scores improved after treatment (P<0.05) and the post-treatment SAS, SDS, and PSQI scores of the observation group were better than those of the control group (P<0.05). Only 5-HT levels were downregulated in the control group after the treatment (P<0.05). Levels of 5-HT, NPY and CGRP were downregulated in the observation group after the treatment (P<0.05). All three indicators were lower in the observation group than those in the control group after the intervention (P<0.05).
The results indicate that acupuncture is an effective treatment modality for patients with IBS-D. Patients interested in acupuncture for the treatment of IBS are encouraged to consult with local licensed acupuncturists to learn more about treatment options.
References
1. Liu ZH, Qi AZ,Li ZR et al. Pathological analysis of Irritable Bowel Syndrome in Chinese Medicine [J] Shaanzi Journal of TCM,2005,26(9):974–975.
2. Li GY. Clinical Observation of Acupuncture-moxibustion in Treating Irritable Bowel Syndrome [J] Shanghai Journal of Acupuncture and Moxibustion, 2018, 37(2):187–191.
3. Drossman DA. The functional gastrointestinal disorders and the Rome Ⅲ process[J]. Gastroenterology, 2006,130 (5):1377-1390.
4. Chinese Society of Traditional Chinese Medicine Branch of the Spleen and Stomach. Consensus on Diagnosis and Treatment of Irritable Bowel Syndrome [J] China Journal of Traditional Chinese Medicine and Pharmacy, 2010,25(7):1062-1063.
5. Zheng XY. Guiding Principles of Clinical Research on New TCM Drugs (Trial) [S].Beijing: China Medical Science and Technology Publishing House,2002:139-143.
6. Kong SP,Wang WQ,Xiao N,et al. Clinical Study on Diarrhea-Predominant Irritable Bowel Syndrome Treated by Acupuncture and Ginger Moxibustion [J]. Shanghai Journal of Acupuncture and Moxibustion,2014,33(10):895-898.


