Acupuncture and cupping are safe and effective treatments for lumbopelvic pain during pregnancy. Researchers conducted an observational study at a hospital-based community antenatal clinic in New Zealand and determined that acupuncture produces significant positive patient outcomes, including reductions in lumbopelvic pain levels. [1] Lumbopelvic pain is in the lower torso, lower back, and pelvic girdle and is frequently experienced by pregnant women. Acupuncture provides an important alternative treatment option because many common prescription drugs and over-the-counter analgesics are not recommended during pregnancy.
During the study period, a total of 245 pregnant women attended the clinic, 144 (56.5%) of whom reported lumbopelvic pain as their primary or secondary complaint. Sixty-three women were excluded from the study as they either did not complete a baseline assessment or did not complete a post-treatment follow-up. Data from 81 women were included in the results. Of the women involved in the study, 45 were nulliparous (55.5%). The majority of women were in the third trimester of pregnancy (49.3%), 31 were in the second trimester (38.2%), and 10 were in the first trimester (12.3%). Most of the women were referred to the clinic by a midwife (72%).
Treatment Approach
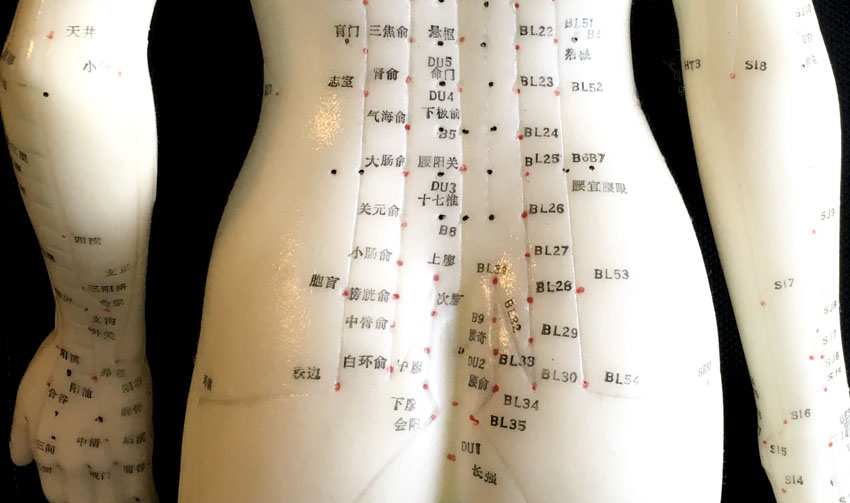
Acupuncture and cupping treatments were provided according to the principles of traditional Chinese medicine (TCM). Points were selected on an individual basis and not all points were used on all of the women. The most commonly used points were Yanglingquan (GB34) and Zulinqi (GB41), which were used in over 50% of all women. Ashi points on the lower back were used in 25–50% of the women, excluding direct needling of Ciliao (BL32) and Zhongliao (BL33). Ashi points surrounding Huantiao (GB30) and ashi points on, near, or between Qiuxu (GB40), Shenmai (BL62), and Taichong (LV3) were also used in 25–50% of women. Ashi points between Neiting (ST44) and Lidui (ST45) and ashi points on, near, or between Chengshan (BL57), Feiyang (BL58), Yintang (MHN3), Baihui (GV20), Kunlun (BL60), Fengshi (GB31), and Waiguan (TB5) were used in fewer than 25% of women. Additionally, cupping therapy to the lower back was provided to over 50% of women in taking part in the study. This is an interesting selection given that cupping is ordinarily contraindicated on the abdomen and lower back during pregnancy.
Upon insertion of the needles, deqi was obtained manually and needles were retained for 20 minutes. Treatment was given once weekly, with each woman receiving a minimum of three treatments. The mean number of treatments was 3.85. Ear press needles were also offered to the women to place on the foot acupoints if desired. They were advised to retain these for 2–3 days and to remove them if they became uncomfortable or itchy.
Results and Discussion
All women taking part in the study completed the Measure Yourself Medical Outcome Profile (MYMOP) questionnaires prior to and after acupuncture treatments. The MYMOP questionnaire allowed the participants to describe their symptoms in their own words and to rate them using a scale of 0–6. They were also allowed to give additional information about other symptoms, especially those related to functional impairment and general well-being. Symptomatic changes were calculated by subtracting the post-treatment score from the pre-treatment score, and a reduction of one point or more was considered clinically significant.
Of the 81 women included in this study, 18 reported an improvement in symptoms of 1–1.99 points (22.2%), 30 reported an improvement of 2 –2.99 points (37.0%), 15 reported an improvement of 3 –3.99 points (18.5%), and 9 reported an improvement of 4 points or more (11.1%). A total of 72 women (88.9%) reported clinically significant improvements following treatments with acupuncture and cupping. The data demonstrates that acupuncture and cupping are effective treatment options.
Related Research
In a prior study conducted at Yale-New Haven Hospital, researchers find auricular acupuncture effective for the treatment of pregnancy-related lower back and posterior pelvic pain. [2] A total of 152 pregnant women completed the study. They were randomized to receive auricular acupuncture, sham auricular acupuncture, or no treatment. All women were 25–38 weeks pregnant and had no prior experience with acupuncture.
Auricular Acupuncture
Auricular press needles were administered at three points (kidney, analgesia, and Shenmen) and were secured with tape. These points were selected for their location close to the hip and lumbar spine areas on the auricular somatotopic map. The participants were instructed to keep these press needles in place continuously for one week without pressing or stimulating them in any way. If they experienced any redness or irritation, they were instructed to return to the clinic to have the needles inspected, adjusted, or removed if necessary.
Sham Auricular Acupuncture
The above procedure was also followed for the sham auricular acupuncture group, with the exception that three non-specific auricular points (shoulder, wrist, extra-auricular) were selected.
Results
Pain and functional status were measured using a Visual Analogue Scale (VAS) with measurements taken at baseline, on day 7, and on day 14. On day 7, all participants reported improvements in pain, with the acupuncture group experiencing the greatest improvements compared to sham and control. In the acupuncture group, 81% of participants experienced significant improvements compared with 59% and 47% in the sham and control groups respectively. Additionally, 37% of women in the acupuncture group were pain-free at the 7-day mark, compared with 22% and 9% in the sham and control groups respectively. One limitation of the study design is that the data may indicate and active sham control, with the shoulder, wrist, and extra-auricular ear acupuncture points potentially providing clinically significant contributions to symptomatic relief.
At the 14 day follow-up, 68% of women in the acupuncture group reported significant improvements in pain levels, with 16% being entirely pain-free. In the sham group, 32% of women saw improvements in pain, with 9% being pain-free. In the control group, 18% had improvements, with 6% being pain-free. The results indicate that auricular acupuncture provides significant clinical benefits.
Author Information:
1. Department of Human Development, Washington State University Vancouver, Vancouver, Washington, USA.
2. National Institute of Complementary Medicine at University of Western Sydney, Sydney, Australia.
3. New Zealand School of Acupuncture and Traditional Chinese Medicine, Wellington, New Zealand.
4. Department of Anesthesiology, Yale School of Medicine, New Haven, Connecticut.
5. Department of Epidemiology and Public Health, Yale School of Medicine, New Haven, Connecticut.
6. Department of Orthopedics and Rehabilitation, Yale School of Medicine, New Haven, Connecticut.
7. Department of Obstetrics and Gynecology, Yale School of Medicine, New Haven, Connecticut.
8. Women's Education and Life Learning Center, Yale-New Haven Hospital, New Haven, Connecticut
9. Departments of Anesthesiology, Pediatrics, Psychiatry, and Human Behavior, University of California School of Medicine, Irvine, California.
References:
1. Soliday E. Betts D. “Treating Pain in Pregnancy with Acupuncture: Observational Study Results from a Free Clinic in New Zealand” Journal of Acupuncture and Meridian Studies 2018;11(1):25e30.
2. Wang S.M. et al. “Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study” American Journal of Obstetrics & Gynecology September 2009.


