A new investigation of acupuncture connects modern research with the traditional inducement of de-qi, a sensation evoked by acupuncture needles. 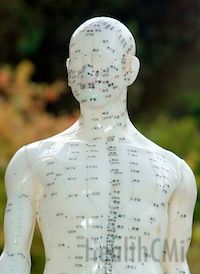 Researchers from Beijing University of Chinese Medicine, Medimar International Hospital and the European Foundation of TCM performed a research meta-analysis of the medical implications of evoking de-qi. Prominent acupuncturists and modern research was included in the study. The findings suggest a direct correlation between ancient acupuncture techniques and improved clinical outcomes for patients.
Researchers from Beijing University of Chinese Medicine, Medimar International Hospital and the European Foundation of TCM performed a research meta-analysis of the medical implications of evoking de-qi. Prominent acupuncturists and modern research was included in the study. The findings suggest a direct correlation between ancient acupuncture techniques and improved clinical outcomes for patients.
A total of 140 acupuncturists were chosen for the study and a publication review of 81 sources met the inclusion criteria out of a total of 352 publications reviewed. The investigators started with a historical account of classical acupuncture and then covered responses by modern clinicians and research. The researchers noted that, historically, The Yellow Emperor’s Inner Canon discussed de-qi but the arrival of Qi was viewed in terms of the practitioner’s experience and not the sensations experienced by the patient. They noted that by the end of the Ming Dynasty, de-qi was described as dull, numb, distention, outward spreading and other similar sensations as described in The Inner Chapters of Acupuncture and Moxibustion.
Modern research was conducted to survey patient responses to de-qi evoked by acupuncture needling. The subjective responses by patients included descriptors such as soreness, dull pain, heat, cold, heaviness, electrical, distention and numbness. The researchers also noted a distinction in subjective responses that were experienced as either fast or slow. Dull aches, for example, had a spreading sensation at a slow rate whereas electrical sensations were rapid. Correlates were drawn between the sensations and the rapid speed of nerve transmission and the slow speed, in centimeters per second, of channel transmission. Prominent acupuncturists added that de-qi is visually observable when the skin surrounding the needle appears tensed, bulged or pitted. The de-qi researchers note that classical authors describe de-qi as both tightness and heaviness that can be perceived in the fingers of the licensed acupuncturist holding the needle.
Acupuncture Speed Unique
The issues of de-qi and speed of transmission has emerged in other independent research. Dr. Jones and Dr. Bae of the University of California, Irvine, delineated three pathways by which acupuncture sends signals to the brain by using fMRI and ultrasound measurements. A very fast bioelectric signal is triggered at acupuncture points that is less than or equal to 0.8ms, another signal travels along nerve pathways and arrives at the brain in 180 - 200ms and a very slow signal arrives at the brain in 15 - 25 seconds as measured from stimulation of acupuncture point UB67 on the foot. The very slow signal travels at a rate of 5 - 10 cm per second. The stimulation process communicates to other acupuncture points along the meridian at this rate and is quantifiable with ultrasound and fMRI measurements. Dr. Jones noted that the very fast 0.8ms response is two orders of magnitude faster than any other known process. If a non-acupuncture point is stimulated, this rapid response is not observed. If one stimulates a true acupuncture point, the speed is less than or equal to 0.8ms, which is not only fast but unequalled at any other area of the body. Only acupuncture points carry information at this rate. The work of Dr. Jones and Dr. Bae relates to this new de-qi research in that the new de-qi research involves a discussion of de-qi and its relationship to neuro-stimulation, perception of de-qi speed sensations and clinical outcomes.
The de-qi researchers uncovered controversy in the determination of de-qi arrival. Dr. Jin R., a prominent acupuncturist, notes that patient sensations of numbness, heaviness and distention are sometimes superficial local sensations and are not necessarily indicative of de-qi. The researchers also noted that “clinical practice has shown that some patients can also get a good efficacy with weak needling sensation or even with no needling sensation at all.” They cited several styles of acupuncture that do not require a needle sensation response to achieve clinical results including abdominal acupuncture, wrist-ankle acupuncture and intradermal needle acupuncture.
Acupuncture Needle Techniques
The research focused on clinical data and licensed acupuncturist input as to the relationship between the arrival of de-qi and specific clinical techniques. Dr. Peng J.S. notes that different de-qi sensations are more appropriate for different ages and body constitutions. Dr. Qiu M.L. notes that changing the direction of needling sensation at one acupuncture point results in specific results. For example, if CV12 is used for the treatment of stomachache, the needle sensation is one of scattering around the region in order to relieve pain. To treat vomiting, the needling sensation is focused downward. Dr. Yu S.Z. notes that evoking numbness and electrical needle sensations are effective in the treatment of excess syndromes and acute diseases. Dr. Guan Z. H. added that needling GB30 for sciatica results in positive patient outcomes when the needle sensation spreads downwards towards the foot.
Various other factors were reviewed in the research including optimum needle retention time and its relationship to de-qi, the quantity of de-qi stimulus, the quality of de-qi stimulus and appropriate techniques to apply after the arrival of de-qi based on needle responses detected by the acupuncturist. Secondary responses to the arrival of de-qi were also reviewed in this meta-analysis and interview process.
There was agreement that secondary responses after the arrive of de-qi that are fierce, unsmooth, difficult for the patient to tolerate or even make the needle physically difficult to manipulate are indicative of a pernicious influence, Xie Qi. However, if the secondary response “comes slowly and softly” as described in the The Yellow Emperor’s Inner Canon, then it is indicative of upright Qi. Dr. Qiu M.L. noted that Xie Qi may involve patient disorders such as acute pain, gallstones, high fever or spasticity. These involve a tense body condition and may lead to a fierce body response after de-qi arrival thereby giving rise to sensations of tenseness, dullness and pain beneath the needle. He noted that upright Qi secondary responses to de-qi are sometimes indicative of symptomatic relieve caused by the acupuncture needle insertion wherein the needle sensation is soft, constant and is “neither of tension nor emptiness.” Dr. Tian C.H. summarized by noting that upright Qi is mild and Xie Qi is quick and tense. The research then turned to a discussion of the specific nerve fibers related to specific de-qi responses.
Interesting feedback by prominent acupuncturists involved a discussion of de-qi and the appropriate acupuncture needle manipulations relative to the responses. There was agreement that the reinforcing and reducing methods can only proceed after the arrival of de-qi. Dr. Jin R. noted that when the Qi arrives slowly there is a sensation beneath the needle of gradually filling and this indicates upright Qi. This indicates the proper application of the reinforcing technique. A compact and fast sensation during the arrival of Qi indicates Xie Qi and therefore a reducing method is appropriate. Dr. Zhang S.C. noted that reinforcing and reducing methods are limited to patient examination and evaluation. Dr. Lu S.Y. added that de-qi sensations often reflect the proper application of the reinforcing and reducing techniques. He noted that the “reinforcing method requires the sensation beneath the needle to be tense and full, which was loose and puff before the procedure. Reducing method requires the unsmooth and tight sensation beneath the needle to be changed.”
Not Just Nerves
This de-qi research coincides with the release of other research finding no correlation between direct nerve stimulation at acupuncture point regions and de-qi sensation. An interesting finding, direct needle stimulation and contact of the median nerve at acupuncture point P6 does not necessarily stimulate a de-qi sensation. Conversely, de-qi is often achieved at P6 without any direct simulation of the median nerve. This and other research finds that de-qi is not caused by direct irritation of a nerve fiber. Rather, de-qi is a physiological response by the central and peripheral nervous system independent of direct contact to nerve fibers. In the same study it was found that achieving de-qi at acupuncture points elicits distinctly different cortical responses than at non-acupuncture points. The researchers suggest that much of these findings point to de-qi having a different effect on the central nervous system dependent on the acupuncture points chosen. Specific acupuncture points demonstrate a consistent and unique ability to stimulate specific brain regions upon de-qi stimulation.
References:
Chen, Sheng, Shengnan Guo, Federico Marmori, Yanping Wang, Qi Zhao, Baokai Wang, Eunhae Ha et al. "Appraisal of the De qi Concept among Contemporary Chinese Acupuncturists."
Zhu, Shi-Peng, Li Luo, Ling Zhang, Song-Xi Shen, Xiao-Xuan Ren, Meng-Wei Guo, Jia-Min Yang et al. "Acupuncture DE-qi: from Characterization to Underlying Mechanism."

