Acupuncture News and Research
- Details

Acupuncture is effective for the treatment of Bell’s palsy, a type of facial paralysis. Researchers at the Anhui Provincial Hospital of Traditional Chinese Medicine conducted an fMRI study analyzing the effects of acupuncture for the treatment of Bell’s palsy. Based on the data, the researchers conclude that acupuncture increases functional connectivity within the sensorimotor cortex and promotes brain reorganization in Bell’s palsy patients. [1] The researchers note that acupuncture directly restores neurosynaptic function and improves positive patient outcomes.
- Details

Acupuncture promotes the healing of bone fractures. Two independent investigations confirm that the addition of acupuncture to usual care protocols increases positive patient outcomes rates. Researchers find acupuncture effective for assisting in the restoration of mobility and reductions in both pain and inflammation.
- Details
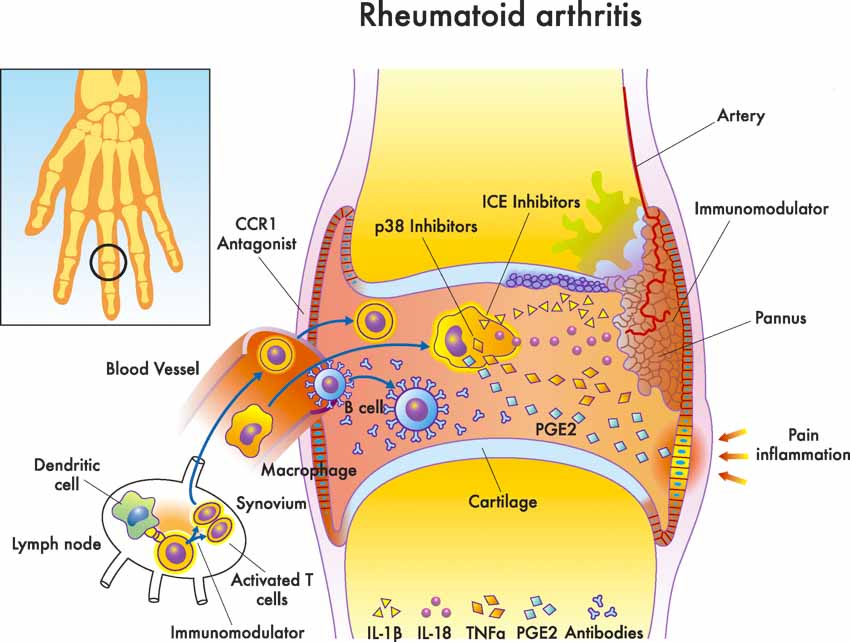
Acupuncture is an effective treatment modality for the the alleviation of rheumatoid arthritis. Researchers conclude that acupuncture alone or in combination with additional treatment modalities alleviates rheumatoid arthritis, restores bodily functions, and improves quality of life. [1] In a meta-analysis, the researchers note that acupuncture exerts its effective actions through several biological mechanisms. The acupuncture research indicates that acupuncture produces anti-inflammatory, antioxidative, and immune system regulatory actions.
- Details

Acupuncture is an effective treatment modality for patients with COPD (chronic obstructive pulmonary disease), an inflammatory lung disease. First Clinical Medicine College of Hubei University of Traditional Chinese Medicine researchers conducted a controlled clinical trial comparing acupuncture with the drug Seretide for improvements in lung function, clinical symptoms, and quality of life for patients with chronic obstructive pulmonary disease. Acupuncture produced results rivalling that of Seretide (a steroid plus beta-2-agonist inhaler). Spirometer measurements document that the lungs improve significantly from the drug and from acupuncture. Acupuncture monotherapy produced significant improvements in forced expiratory volume (FEV1), FEV1 to forced vital capacity ratio (FEV1/FVC), and peak expiratory flow (PEF). [1]
- Details
Researchers find acupuncture effective for the treatment of coronary heart disease (CHD). Using Single Photon Emission Computed Tomography (SPECT) scans, researchers from the Department of Nuclear Medicine at Peking University Shenzhen Hospital document that acupuncture produces a 70.1% blood perfusion improvement in ischemic myocardium CHD patients, while sublingual administration of nitroglycerine produces a 77.4% improvement. [1] The SPECT scans indicate that acupuncture produces clinically significant results.
- Details
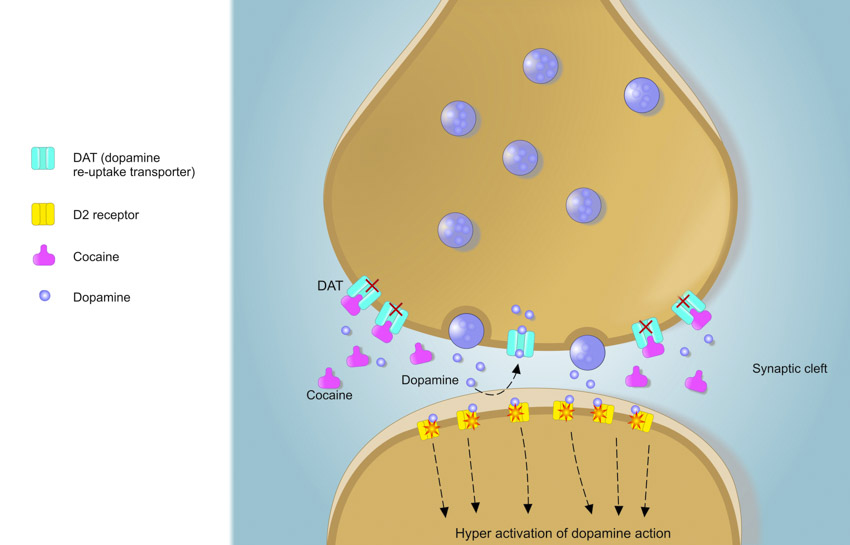
Acupuncture regulates cocaine seeking behavior. University researchers document that acupuncture suppresses addictive behavioral and neurochemical changes caused by cocaine intake. In a controlled laboratory experiment, researchers have documented a specific acupuncture point that blocks deleterious cocaine induced changes. Specifically, application of acupoint HT7 (Shenmen) suppresses cocaine’s stimulation of increases “in locomotor activity and the expression of pCREB and c-Fos in the NAc.” [1]
- Details
Acupuncture is effective for the prevention of acute myocardial ischemia (AMI), a condition causing damage to the heart from reduced cardiac blood flow and oxygen deprivation. Anhui University of Traditional Chinese Medicine researchers conclude that acupuncture applied to acupoints Shenmen (HT7) and Tongli (HT5) protects myocardial cells from ischemic injuries. In a laboratory experiment, the university researchers have proven that acupuncture prevents myocardial ischemia by regulating pro-inflammatory factors and hippocampal neurotransmitters. [1] The researchers note, “Electroacupuncture can protect myocardial cells in AMI rats, which may be associated to its effect in inhibiting the expression of serum creatine kinase (CK), hippocampal norepinephrine (NE), interleukin 6 (IL-6), interleukin-1β (IL-1β), and tumor necrosis factor- alpha (TNF-α).”
- Details

Acupuncture news releases received a great deal of attention at HealthCMi this summer. The following are short excerpts taken from the HealthCMi summer top three list. The first in our top three is an article on the topic of acupuncture for the treatment of neck pain due to disc degeneration.
- Details
Acupuncture alleviates depression and cravings associated with alcohol dependence. Affiliated Hospital of Henan Institute of Traditional Chinese Medicine researchers conducted a controlled clinical trial quantifying changes in alcohol cravings and depression levels using the Hamilton Depression Rating Scale (HAMD) and the Visual Analog Scale (VAS). Two groups were compared. One group received Traditional Chinese Medicine (TCM) emotional reconciliation therapy. Another group received TCM emotional reconciliation therapy plus acupuncture. The results demonstrate that the combination of acupuncture with TCM emotional reconciliation therapy is effective for the alleviation of depression and cravings in patients with alcohol dependency.
- Details

Acupuncture combined with herbal medicine benefits children with autism. Hebei Province researchers conducted a clinical trial and determined that acupuncture and herbal medicine treatments produce significant clinical benefits. The researches conclude that acupuncture improves communication, language, physical movement, and sensory perception. In addition, the children in the study demonstrated improvements in self-care. Based on the data, the researchers conclude that the addition of acupuncture and herbal medicine to a standard rehabilitation protocol improves positive patient outcomes.
- Details

Acupuncture combined with topical herbs is effective for the treatment of facial paralysis. Researchers from the Traditional Chinese Medicine department of People’s Hospital (Huairen, Shanxi) tested two acupuncture protocols. Using acupuncture as a monotherapy produced a 76.92% total effective rate. The addition of topical herbal medicine to the acupuncture point prescription increased the total effective rate to 97.44%. [1] The type of facial paralysis examined in the investigation is categorized as Bell’s palsy.
- Details
Guangzhou University of Traditional Chinese Medicine researchers find two different styles of acupuncture effective for the alleviation of knee osteoarthritis. Patients in the clinical trial had significant reductions in pain, stiffness, and joint immobility. The two styles tested were conventional acupuncture and four seas acupuncture. Results were very similar when comparing both groups. Four seas acupuncture produced a 96.7% total effective rate. Conventional acupuncture produced a 93.3% total effective rate. [1]
- Details

Acupuncture alleviates migraine headaches. Many clinical trials compare MRI scans, biological markers, and subjective clinical outcomes in human trials. This investigation varies by using only biological markers to confirm the results in a laboratory investigation. Overall, this multi-arm investigation demonstrates that a limited acupuncture point prescription of local points is enhanced by the addition of distal acupoints.
- Details
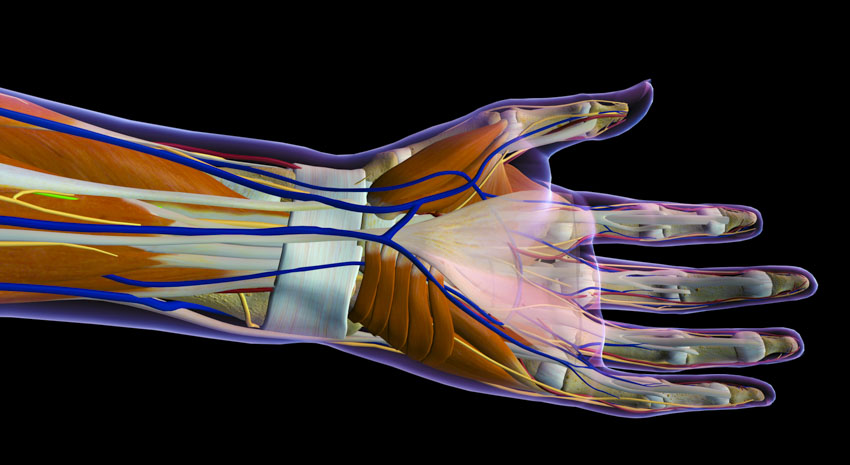
Researchers find acupuncture effective for the treatment of carpal tunnel syndrome (CTS), a local entrapment neuropathy affecting the wrist and hand that causes pain, numbness, and dysfunction. The research team documents acupuncture’s beneficial influence on the morphology of the median nerve and improvement of clinical symptoms.
- Details

Acupuncture alleviates osteoporosis related pain and improves bone mineral density. First Affiliated Hospital of Chengdu Medical College researchers conducted a controlled clinical trial. The team measured bone mineral density and serum osteocalcin before and after the study, along with visual analog scale (VAS) measurements of pain levels. Based on the scientific evidence, the researchers conclude that acupuncture reduces pain levels and promotes increased bone density in patients with osteoporosis. [1]
- Details
Acupuncture helps to heal peptic ulcers and prevents relapses. Researchers conclude that acupuncture increases the total effective rate of drug therapy for the treatment of peptic ulcers. Researchers from the Second Affiliated Hospital of Zhongnan University (Hunan, China) combined acupuncture with standard drug therapy. Patients receiving both drug therapy and acupuncture in a combined treatment protocol had superior patient outcomes compared with patients receiving only drug therapy. Furthermore, acupuncture increases the H. pylori-negative conversion rate and decreases the recurrence rate of drug therapy. [1] In a significant finding, acupuncture added to usual care reduces the relapse rate from 41.7% to 15.4%.
- Details

Dalian Hospital of Traditional Chinese Medicine researchers confirm that acupuncture combined with herbal medicine is effective for the treatment of insomnia in Parkinson’s disease patients. In a controlled clinical trial, a combination of scalp acupuncture and a modified version of the herbal formula Gui Pi Tang were tested. Using the Pittsburgh Sleep Quality Index (PSQI) as a quantitative measure, Parkinson’s disease patients demonstrated significant improvements in sleep. [1]
- Details

Acupuncture continuing education requirements have changed within Texas and the proposed changes to California requirements have not been implemented yet. However, the NCCAOM (National Certification Commission for Acupuncture and Oriental Medicine) has announced a special cooperative agreement for licensed acupuncturists in California. Let’s take a look at the changes.
- Details
Acupuncture and cupping are safe and effective treatments for lumbopelvic pain during pregnancy. Researchers conducted an observational study at a hospital-based community antenatal clinic in New Zealand and determined that acupuncture produces significant positive patient outcomes, including reductions in lumbopelvic pain levels. [1] Lumbopelvic pain is in the lower torso, lower back, and pelvic girdle and is frequently experienced by pregnant women. Acupuncture provides an important alternative treatment option because many common prescription drugs and over-the-counter analgesics are not recommended during pregnancy.
- Details

Acupuncture is an effective treatment modality for the alleviation of fibromyalgia. Researchers at the Physical Medicine and Rehabilitation Department of Ataturk University conclude that acupuncture improves two biochemical markers and clinical outcomes for patients with fibromyalgia. Objective measures show that acupuncture increases serum serotonin levels while simultaneously reducing Substance P levels. For subjectives, the researchers document lasting subjective improvements including less pain, fatigue, and anxiety. [i]

