Acupuncture News and Research
- Details
Researchers tested the efficacy of acupuncture and herbal medicine for the treatment of diabetic peripheral neuropathy. All participants in the clinical trial were provided usual care. An observation group was provided additional therapeutics with acupuncture and Chinese herbal medicine. The addition of acupuncture and herbal medicine to usual care improved overall outcomes by 7.5% and the acupuncture and herbal medicine group had significantly greater outcomes for improvements in nerve conduction velocity. [1]
- Details
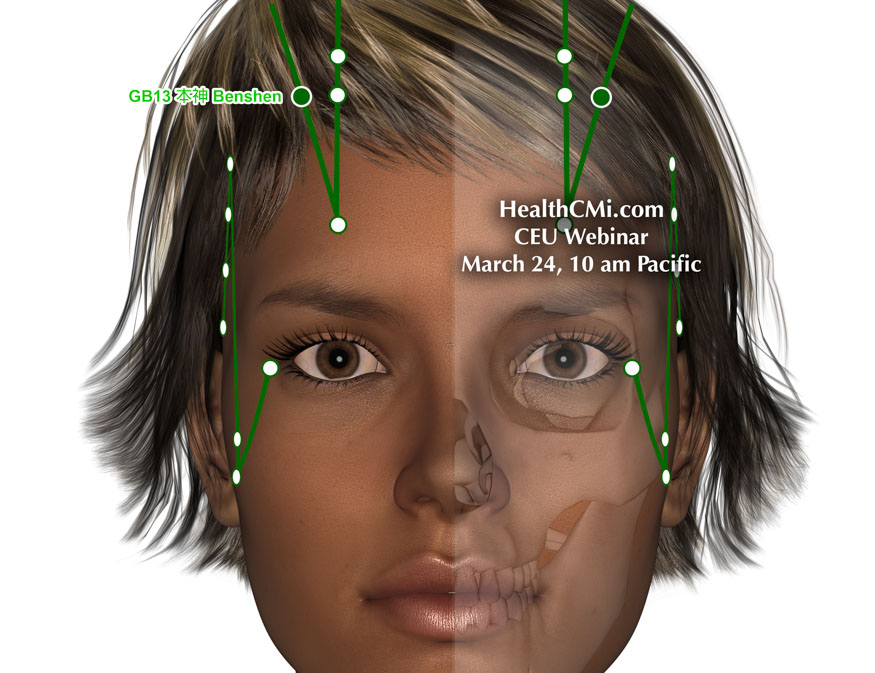
HealthCMi is airing a live acupuncture CEU webinar featuring the treatment of anxiety, hypertension, and fibromyalgia. This live webinar airs on Sunday, March 24th at 10 am Pacific Time. This webinar is acupuncture board approved for every state in the USA, including CEUs from the California Acupuncture Board, Texas State Board of Acupuncture Examiners, CTCMA (British Columbia, Canada), NZASA & Acupuncture NZ (New Zealand), NCCAOM, and many more.
- Details
Researchers find acupuncture effective for the alleviation of delayed menstruation. Two acupuncture treatments were compared, and one of the approaches to patient care produced optimal results. The researchers defined delayed menstruation as a menstrual cycle that is postponed by more than seven days (sometimes extending to 40–50 days) for two or more consecutive cycles. They classified this under the dysfunctional uterine bleeding category and add that late menstrual periods in Chinese medicine are often due to liver qi stagnation syndrome or qi and blood deficiency.
- Details

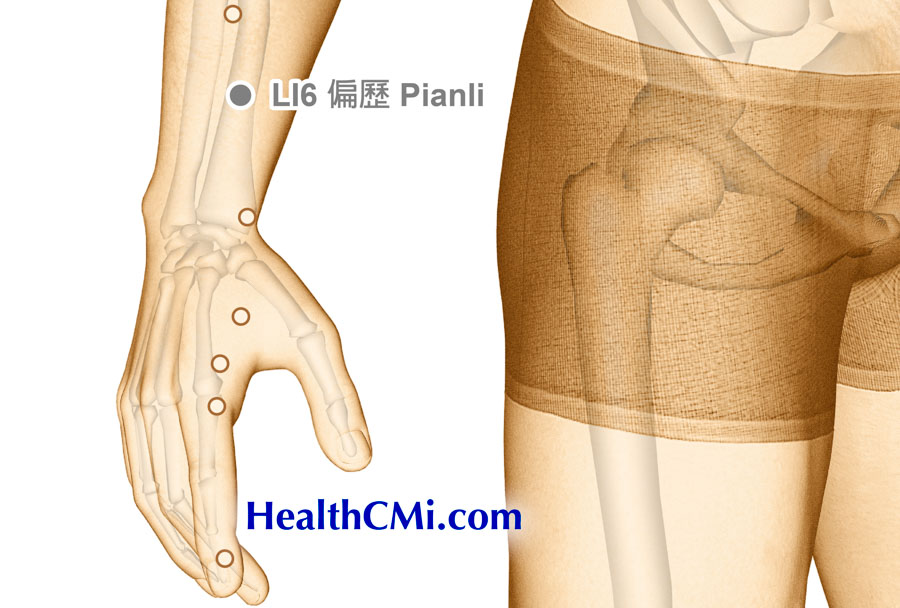
HealthCMi is airing a live acupuncture CEU webinar on the treatment of back pain and carpal tunnel syndrome. This live webinar airs on Sunday, March 17th at 10 am Pacific Time. A look at specific acupuncture points confirmed by modern research compares the efficacy of different approaches to patient care. The event covers a type of triple acupuncture that significantly promotes pain relief and recovery.
- Details

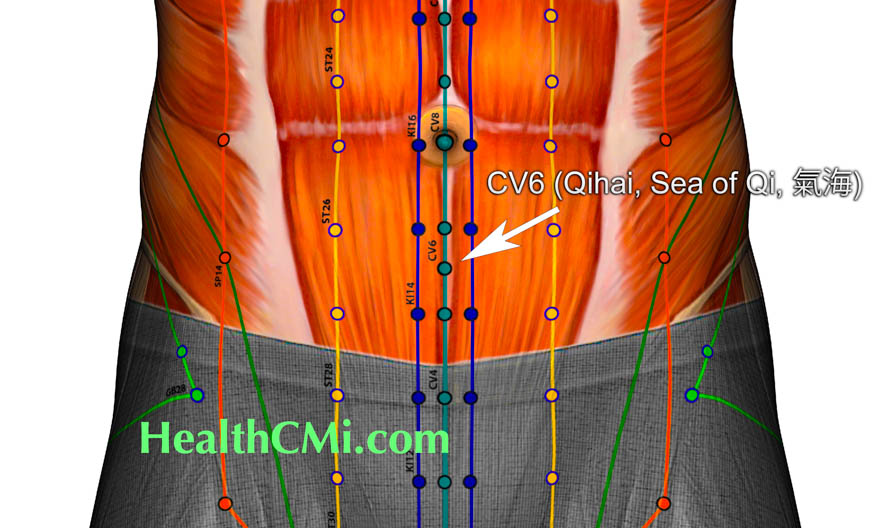
Researchers have tested and confirmed an effective acupuncture treatment for patients with functional dyspepsia (chronic upset stomach). Functional dyspepsia is characterized by a recurring upset stomach of unknown or unspecified cause. It is non-ulcerative; however, it mimics ulcerative stomach disorders. There is recurring upper abdominal pain or discomfort, often with bloating, nausea, or belching. There may be postprandial fullness or early satiation, without a clear structural cause.
- Details
Researchers find acupuncture an effective treatment modality for the alleviation of eczema (atopic dermatitis). Chronic eczema, a common dermatological condition encountered in clinical practice, presents a certain level of treatment difficulty, often accompanied by severe itching that significantly impacts patients' quality of life. The etiology of chronic eczema is complex, making the condition persistent and recurrent.
- Details

HealthCMi is airing a live acupuncture CEU webinar on the treatment of anxiety, depression, and insomnia. This special event starts Sunday, March 3rd at 10 am Pacific Time. Recent developments in acupuncture research are presented showing the relationship between medical efficacy and specific acupuncture point prescriptions. Clinical and laboratory research, along with Chinese medicine principles, demonstrate modern enhancements in patient care for optimizing results. A special focus is on moving qi circulation to enhance relaxation.
- Details

Acupuncture is effective for the treatment of PTSD, especially in combat veterans. In a high-quality placebo controlled clinical trial, researchers conclude that true acupuncture produces moderate to large beneficial clinical and biological outcomes for combat veterans with PTSD. Improvements were significant for the reduction of overall symptom severity and for large scale extinction of fear and startle responses. [1]
- Details

Acupuncture has been shown effective for the management of high blood pressure. Researchers compared the efficacy of captopril with the use of three specific acupoints. The acupoint combination outperformed the medication control group by 14%.
- Details
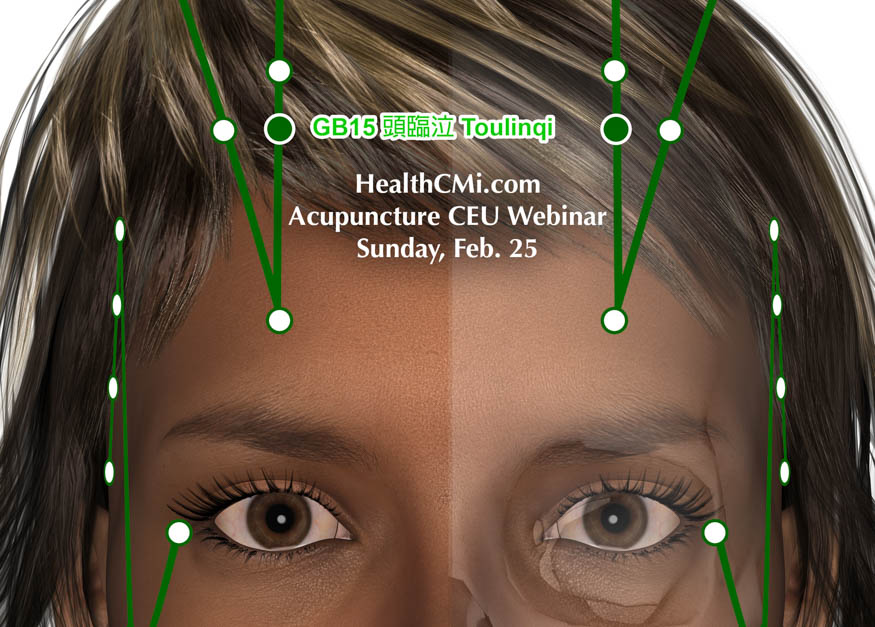
HealthCMi airs a live acupuncture CEU webinar on headache and depression relief, featuring acupuncture points proven effective in modern research. This live event is on Sunday, February 25 at 10 am Pacific Time. Participants receive full in-person acupuncture CEU credit in this online webinar. This acupuncture continuing education course is state, national, and international board approved. Explore special acupuncture points and the modern research supporting their use in clinical practice.
- Details

Acupuncture alleviates pain and motor dysfunction of the temporomandibular joint (TMJ). Researchers tested two approaches to clinical care with acupuncture. A combination of manual acupuncture plus electroacupuncture produced optimal outcomes. [1]
- Details
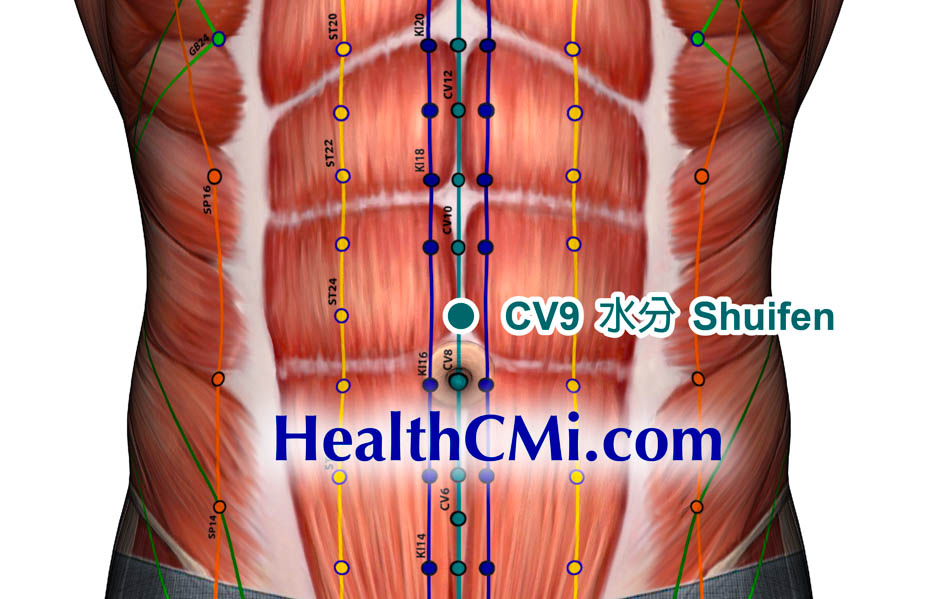
Acupuncture is effective for the treatment of acute exacerbations of chronic obstructive pulmonary disease (AECOPD) accompanied by gastrointestinal dysfunction. A clinical trial conducted by researchers at Chengdu University of Traditional Chinese Medicine involving 100 AECOPD cases compared the effectiveness of enhanced pharmaceutical care with electroacupuncture plus drug therapy. The results of the clinical trial revealed superior patient outcomes with electroacupuncture. [1]
- Details

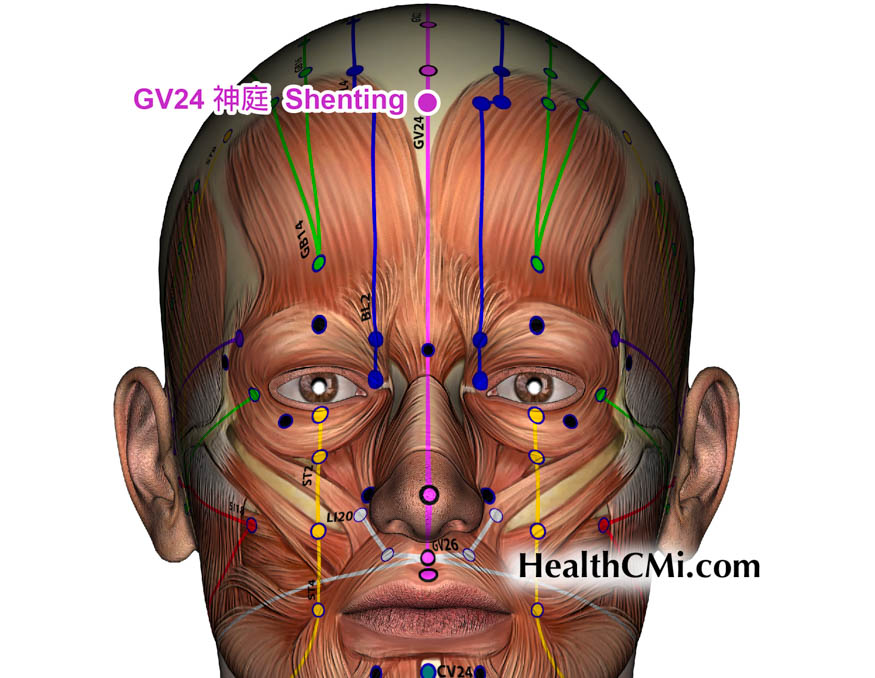
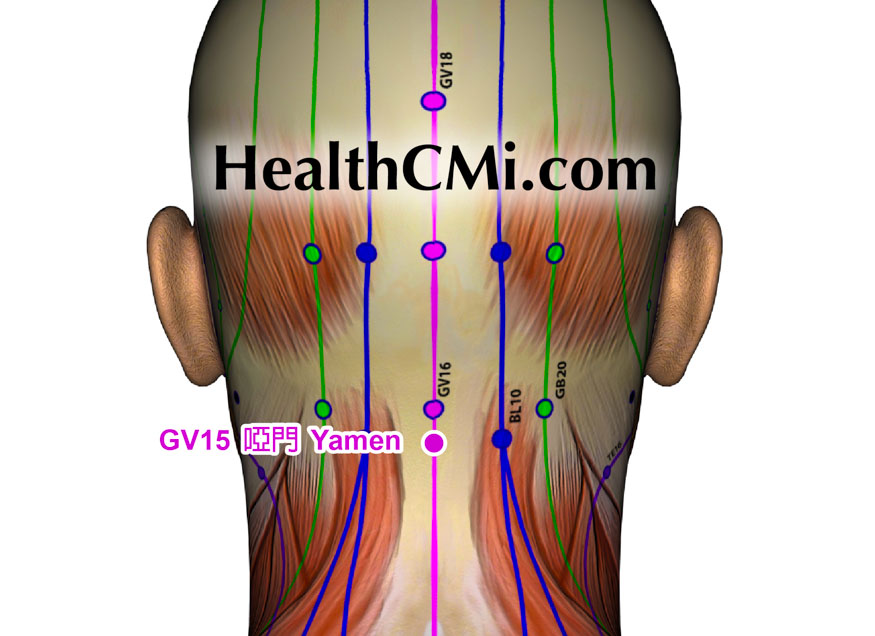
Prof. Richard Liao, L.Ac. has launched an acupuncture continuing education course featuring all governing vessel (du mai) acupuncture points. The course features every governing vessel acupoint, its pathways, meeting points, and more. This course also features modern research showing the efficacy of specific governing vessel acupoints for the treatment of migraines, asthma, pneumonia, lumbar disc herniations, and more.
- Details
Acupuncture and herbal medicine benefit patients with post-stroke aphasia. Researchers determined that patients receiving acupuncture and physical therapy combined with herbal medicine have an 11.57% increase in total efficaciousness over patients receiving only acupuncture and physical therapy. Acupuncture plus physical therapy resulted in an 86.05% total effective rate and acupuncture plus physical therapy combined with herbal medicine prodiuced a 97.62% total effective rate. [1]
- Details

HealthCMi presents a live acupuncture CEU webinar for the treatment of anxiety, hypertension, and shen-spirit acupoints on Sunday, February 11 at 10am Pacific Time. Explore acupuncture points supported by modern research that effectively regulate and lower blood pressure. A special section of the acupuncture continuing education webinar addresses shen-spirit points that benefit the seven emotions. Modern research showing acupuncture and Chinese medicine benefitting patients with heart disease and shen (spirit) disturbances is presented.
- Details

Acupuncture is an effective treatment modality for headaches due to cervical spine and soft tissue disorders. Today, we cover a variety of research showing acupoints used across multiple clinics that demonstrate results in modern research. We start with both ancient writings and modern electroacupuncture to examine the overall effectiveness of acupuncture for this condition.
- Details

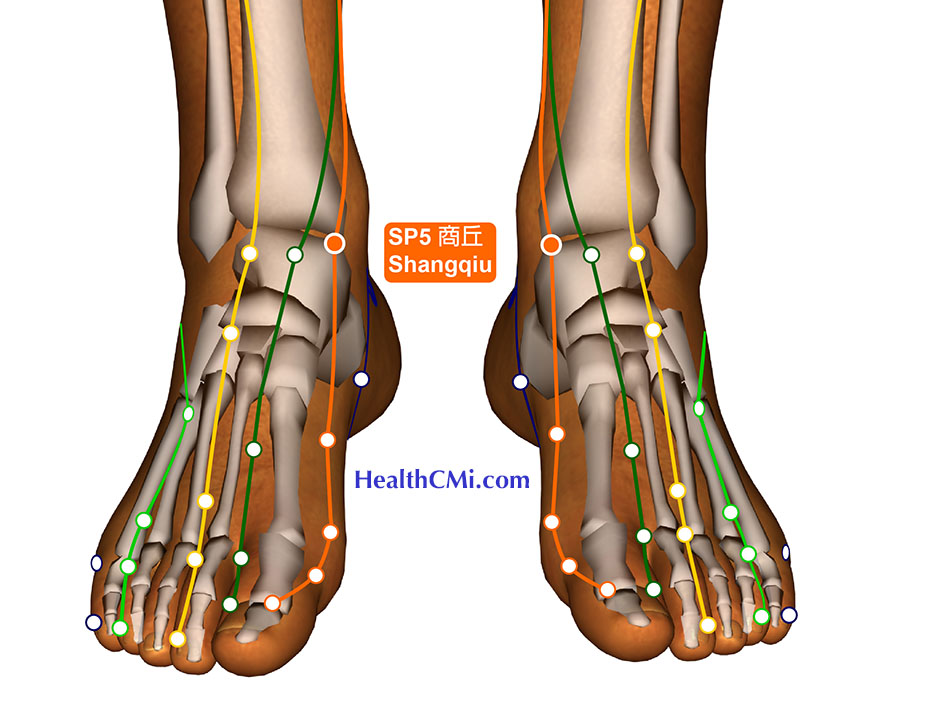
HealthCMi presents a live acupuncture CEU webinar for the treatment of neck and back pain on Sunday, February 4 at 10 am Pacific Time. This webinar covers modern research showing specific acupuncture points that increase endorphin levels in patients with lumbar disc herniations. This webinar also shows research supported acupuncture points that alleviate neck and back pain, including neck pain caused by intervertebral disc degeneration.
- Details

Acupuncture promotes health in patients with postmenopausal osteoporosis. Researchers determined that acupuncture significantly increases positive patient outcomes for postmenopausal patients taking calcium supplementation. Acupuncture increases bone density, reduces pain levels, and improves FSH, LH, E2, IGF-1, TNF-α, and IL-6 blood levels.
- Details
Acupuncture treatment assists patients in alleviating pain and actively dealing with accumulated uric acid. The electroacupuncture method was used to treat patients with gouty arthritis (GA). Researchers at the Orthopedic Department of Malanshan Traditional Chinese Medicine Hospital investigated acupuncture and determined that it helps to stimulate acupoints and regulate meridians, thereby strengthening the body’s defenses. [1]
- Details

Acupuncture improves sleep for Parkinson’s disease patients. Guangzhou University of Chinese Medicine and Dalian University of Technology researchers performed a meta-analysis of 13 randomized controlled trials, comprised of 719 patients. True acupuncture outperformed medication monotherapy and sham acupuncture. Based on the data, the researchers conclude that acupuncture improves sleep quality for Parkinson’s disease patients and may improve psychological and behavioral conditions as well.

