Western Sydney University researchers find acupuncture effective for the alleviation of menstrual pain. The investigation team, led by chief researcher Dr. Armor, finds acupuncture effective for reducing both pain intensity levels and the duration of menstrual cramping and pain. In addition, the researchers document that acupuncture reduces secondary symptoms including back pain, headaches, and nausea. Perhaps more importantly, the beneficial clinical effects were sustained for up to one year after completion of acupuncture treatments.
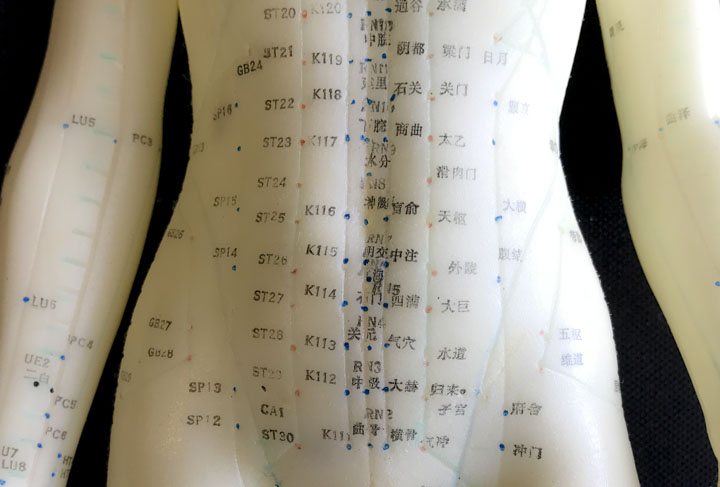
The Australian research team investigated the effects of manual acupuncture and electroacupuncture on patients with chronic dysmenorrhea (menstrual related cramping and pain). All participants received a grand total of 12 acupuncture treatments. Manual acupuncture group participants received tonification (bu) or sedation (xie) methods applied to the acupuncture needles during the 20–30 minute acupuncture sessions. For electroacupuncture participants, “two distal points were selected by the practitioner and a 2Hz/100Hz square wave pulse of 200ms duration was applied between each point for 20 minutes using an ITO ES-160 electroacupuncture machine.”
At the Healthcare Medicine Institute, we have discussed our workbench reviews of the ITO ES-160 electroacupuncture device at several live webinar events. It is notable that the research team used this unit. We find it highly reliable and it offers a sweep mode in addition to the standard alternating current mode. While the compact ES-130 unit tends to be more popular with licensed acupuncturists, the larger and more sophisticated ES-160 offers added features, which may be of benefit to acupuncturists. Please note that the Healthcare Medicine Institute has no financial association with the manufacturer and there is no conflict of interest. Our goal is to provide reporting on quality research, test acupuncture and herbal medicine related equipment, provide reviews of texts, and provide acupuncture continuing education courses online.
The researchers conclude, “This exploratory study suggests acupuncture administered over three menstrual cycles gave both statistically and clinically significant reductions in menstrual pain compared to baseline and persisted for 12 months….” In this study, manual acupuncture slightly outperformed electroacupuncture. The researchers note, “Manual acupuncture provided the same or greater pain relief as electro-acupuncture, but with less analgesic medication required to achieve this pain reduction.”
Additional studies find acupuncture effective for the treatment of dysmenorrhea. Wenqing Wang’s research entitled Clinical Treatment of Primary Dysmenorrhea Using Acupuncture finds acupuncture more effective than ibuprofen. A total of 122 women ranging in ages from 14 to 43 were separated into an acupuncture treatment group, medication group, and a B vitamin nutritional supplement group. All groups received treatment over the course of three menstrual cycles. All groups received treatment for 5 days starting from the day prior to the expected start of menses. The acupuncture group received treatment once per day. The acupuncture points used in the study were the following:
- SP6 (Sanyinjiao)
- SP8 (Diji)
- SP10 (Xuehai)
- LI4 (Hegu)
The medication group received ibuprofen tablets 2–3 times per day and the supplement group received vitamin B supplements. The result showed that the acupuncture group had a significantly higher effective treatment rate (96.2%) compared with the ibuprofen medication group (80%) and the supplement group (13.3%).
Jiao et al. document similar findings and conclude that acupuncture plus moxibustion has a 96.8% total treatment effective rate for the treatment of dysmenorrhea, whereas ibuprofen sustained time release capsules achieved a 58.1% total treatment effective rate. The primary acupoints administered to all patients patients were the following:
- Guanyuan (CV4)
- Zhongji (CV3)
- Sanyinjiao (SP6)
Additional acupoints were selected based on differential diagnostics. For qi and blood stasis, the following acupoints were added:
- Taichong (LV3)
- Xuehai (SP10)
For depressed liver qi with dampness and heat, the following acupoints were added:
- Xingjian (LV2)
- Yinlingquan (SP9)
For liver and kidney deficiency, the following acupoints were added:
- Shenshu (BL23)
- Mingmen (GV4)
For poor qi and blood circulation, the following acupoints were added:
- Qihai (CV6)
- Zusanli (ST36)
Manual acupuncture stimulation techniques for obtaining deqi including lifting, thrusting, and rotating were applied. Once a deqi sensation was obtained, the needles were retained and moxibustion applied to the acupoints via attachment to the needle handle. One acupuncture treatment was administered daily for 3–4 consecutive days during menstruation. Treatment was also conducted on the 2 days prior to the next menstrual cycle. The entire course of treatment comprised 3 menstrual cycles. For the ibuprofen group, patients received 300 mg of ibuprofen sustained time release capsules starting 1 – 2 days prior to menstruation. Capsules were orally administered twice per day for 2 – 3 days until the symptoms were mitigated, for a total of 3 menstrual cycles. Vitamin B was administered additionally for patients who also experienced stomach discomfort. The results tabulated, the acupuncture plus moxibustion protocol provided greater pain relief than the ibuprofen protocol.
References
Mike Armour, Hannah G. Dahlen, Xiaoshu Zhu, et al (2017). The role of treatment timing and mode of stimulation in the treatment of primary dysmenorrhea with acupuncture: An exploratory randomized controlled trial. PLoS ONE 12(7): e0180177.
Wenqing Wang (2007). Clinical Treatment of Primary Dysmenorrhea using Acupuncture. Hubei TCM Magazine, 2007. 29(6): 57.
Liangxi Zhi (2007). Treatment of Primary Dysmenorrhea using Fu’s subcutaneous needle. Chinese Acupuncture, 2007. 27(1): 18-21.
Jiao FL, Liang YC & He M. (2014). Therapeutic Observation of Acupuncture-moxibustion for Primary Dysmenorrhea. Shanghai Journal of Acupuncture and Moxibustion. 33(5).


