Acupuncture alleviates schizophrenia. Harbin First Specialized Hospital (China) researchers determined that acupuncture enhances the effects of the antipsychotic medication clozapine in the relief of refractory schizophrenia. [1] The study compared clozapine combined with acupuncture with clozapine monotherapy. The total effective rate in the acupuncture integrative medicine group was 94.3% compared with 73.3% in the drug monotherapy group. Patients in the acupuncture group experienced fewer adverse effects with a rate of 8.6% compared with 36.7% in the drug monotherapy group. The researchers conclude that acupuncture combined with clozapine is safe, reliable, and worthy of recommendation.
A total of 65 patients diagnosed with refractory schizophrenia were recruited for the study and were randomly assigned to group 1 or group 2. Group 1 was comprised of 15 male and 15 female patients, ages 24–52, years with a disease duration of 4–13 years. Group 2 was comprised of 11 male and 14 female patients, ages 23–53 years, with a disease duration of 3–12 years. There were no significant differences in baseline characteristics between the two groups (p>0.05).
Each patient’s condition was adequately maintained before enrolment into the study. Exclusion criteria included: serious organ damage or pathological changes, inability to tolerate the treatment methods used in the study, intellectual disability, inability to complete the 12-week study period.
Medicine
All participants were prescribed clozapine, an antipsychotic and a drug of choice for the treatment of refractory schizophrenia. All patients were started on a dose of 50 mg, taken morning and evening, in divided doses. The dosage was increased gradually over the course of a week to a maximum of 200–500 mg daily according to the severity of each patient’s symptoms. In addition, the participants in group 2 received acupuncture treatment administered at the following primary acupoints:
- Baihui (GV20)
- Sishencong (MHN1)
- Shangxing (GV23)
- Shuigou (GV26)
- Fengchi (GB20)
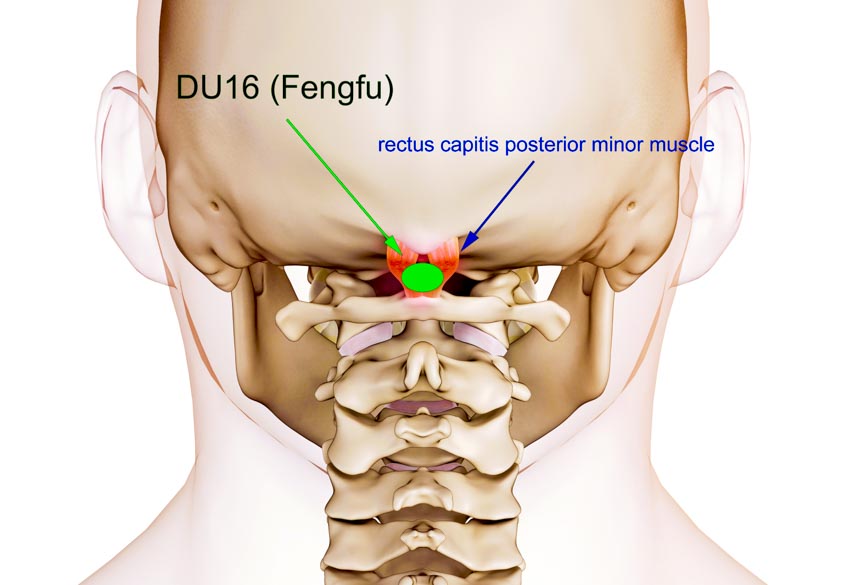
- Fengfu (GV16)
- Hegu (LI4)
- Taichong (LV3)
- Zusanli (ST36)
The following secondary acupoints were added according to each patient’s individual symptoms:
- For patients with auditory hallucinations, Yifeng (TB17), Tinggong (SI19), and Tinghui (GB2) were added.
- For patients with visual hallucinations, Zanzhu (BL2) and Yuyao (MHN6) were added.
- For patients suffering from delusions, Dazhui (GV14) and Taodao (GV13) were added.
Sterile 0.30 × 50 mm needles were selected and inserted. Needles were inserted obliquely into points on the head at a 15-degree angle from the skin, and perpendicularly into points on the limbs at a 90-degree angle from the skin. Needles were retained for 30 minutes and manipulated once during this timeframe. Treatment was administered five days a week with each course consisting of 10 treatments. A total of six courses were administered over 12 weeks.
Results
Outcome measures for the study included the PANSS (Positive and Negative Syndrome Scale), the BPRS (Brief Psychiatric Rating Scale), the total treatment effective rate, and the incidence of adverse effects. The PANSS is a scale designed to assess positive and negative symptoms in schizophrenia and psychosis and is considered a gold standard for gauging the efficacy of antipsychotic medications. Higher PANSS scores are indicative of more severe symptomatology. Before treatment, mean PANSS scores were 97.2 in group 1 and 88.4 in group 2. Following 12 weeks of treatment, these scores fell to 48.5 and 32.4 respectively.
The BPRS is used to assess a range of psychiatric symptoms, including those associated with mood, behavior, mannerisms, unusual thoughts, and hallucinations, etc. Each symptom is rated on a scale of 1–7, with 1 indicating an absence of that particular symptom and higher scores indicating increased severity. Before treatment, mean BPRS scores were 81.2 in group 1 and 80.2 in group 2. Following 12 weeks of treatment, these scores fell to 65.1 and 52.9 respectively. Both groups experienced significant improvements in PANSS and BPRS scores following treatment (p<0.01). Improvements were significantly greater in the acupuncture integrative medicine group (p<0.05).
The total effective rate for each treatment was calculated. In patients with an improvement in BPRS scores of >60%, the treatment effect was classified as excellent. In patients with an improvement in BPRS scores of 20–60%, the treatment effect was classified as good. In patients with improvements in BPRS scores of <20%, the treatment effect was classified as poor. The number of excellent and good cases were added together to give the total effective rate.
In group 1, there were 15 excellent, 7 good, and 8 poor cases, giving a total effective rate of 22/30 (73.3%). In group 2, there were 27 excellent, 6 good, and 2 poor cases, giving a total effective rate of 33/35 (94.3%). The difference between the two groups was considered statistically significant (p<0.01).
Adverse effects were monitored throughout the study. These included symptoms such as elevated heart rate, dry mouth, somnolence, and weight gain. In group 1, 11 patients experienced adverse effects, giving an incidence of 36.7%. In group 2, only 3 patients experienced adverse effects, giving an incidence of 8.6%. The difference between the two groups was determined statistically significant (p<0.01).
The results of this study indicate that acupuncture is a useful adjunct to the antipsychotic medication clozapine for the treatment of refractory schizophrenia. It has the potential to enhance efficacy and reduce the incidence of adverse reactions and is worthy of clinical consideration.
Reference:
1. Liao Yanping (2019) Effect of acupuncture and moxibustion combined with clozapine in the treatment of refractory schizophrenia. Heilongjiang Science Vol.10 (6) pp.50-51.


