Acupuncture provides headache relief. Liaoning University of Traditional Chinese Medicine researchers (Shenyang, China) tested the efficacy of acupuncture in a randomized controlled clinical trial. The researchers determined that acupuncture is both safe and effective for the alleviation of headaches.
The study compared the effects of Traditional Chinese Medicine (TCM) acupuncture with tetrahydropalmatine (THP) and non-acupoint needling in 177 headache patients. The total effective rate was 97.96% in the acupuncture monotherapy group compared with 89.87% in the THP control group. The researchers conclude that TCM acupuncture provides significant therapeutic effects and reduces pain while avoiding the adverse effects associated with medications.
A total of 98 headache patients admitted to the department of TCM were assigned to the acupuncture group and 79 patients admitted to the department of western medicine were assigned to the THP control group. The participants were comprised of 59 male and 118 female patients, ages 18–71 (mean age 41.78 years), with a disease duration between 2 days and 3 years. There were no statistically significant differences in baseline characteristics between the two groups at the outset of the investigation (p>0.05).
Patients assigned to the THP control group were treated with a combination of tetrahydropalmatine (30 mg, three times a day) and non-acupoint needling. Tetrahydropalmatine is an isoquinoline alkaloid extracted from plants, especially from Yan Hu Suo (Corydalis). Patients assigned to the acupuncture group received acupuncture treatment according to TCM pattern differentiations but did not receive any medications. The relevant patterns, symptoms, and acupoints for each headache type were as follows:
Liver and kidney yin deficiency
Symptoms: vertigo, dizziness
Primary acupoints:
- Sanyinjiao (SP6)
- Ganshu (BL18)
- Taixi (KD3)
- Shenshu (BL23)
Secondary acupoints:
- Yuyao (MHN6)
- Zanzhu (BL2)
Wind-heat
Symptoms: fever, aversion to wind, thirst, irritability, nasal congestion
Primary acupoints:
- Waiguan (TB5)
- Taiyang (MHN9)
- Fengfu (GV16)
- Fengchi (GB20)
For frontal headaches, add:
- Shangxing (GV23)
- Yintang (MHN3)
Blood deficiency
Symptoms: palpitations, poor memory, fever, fatigue, insomnia, dry eyes, lack of vitality, pale lips and complexion, anorexia, deep-fine pulse
Primary acupoints:
- Xinshu (BL15)
- Geshu (BL17)
- Pishu (BL20)
- Zusanli (ST36)
Secondary acupoint:
- Qihai (CV6)
Wind-cold
Symptoms: fever, aversion to cold, nasal congestion, watery eyes and nose, anhidrosis, lack of thirst, sore back, temporal, medial, or posterior headache, white-greasy tongue coating, floating-slippery pulse
Primary acupoints:
- Dazhui (GV14)
- Fengfu (GV16)
- Lieque (LU7)
For posterior headache, add:
- Kunlun (BL60)
Qi deficiency
Symptoms: sensation of heat, irritability, aversion to cold, dislike of speaking, anorexia, fatigue, shortness of breath, spontaneous sweating, worsening of symptoms at night, overflowing-big pulse
Primary acupoints:
- Qihai (CV6)
- Guanyuan (CV4)
- Zusanli (ST36)
- Baihui (GV20)
Secondary acupoint:
- Taibai (SP3)
Wind-damp
Symptoms: low-grade fever, aversion to wind, sore joints, sensation of heaviness, generalized pain, dark and scanty urine, symptoms aggravated by wind, greasy tongue coating, floating-moderate pulse
Primary acupoints:
- Fengfu (GV16)
- Dazhui (GV14)
- Fenglong (ST40)
- Touwei (ST8)
Secondary acupoints:
- Sanyinjiao (SP6)
- Yinlingquan (SP9)
Phlegm obstruction
Symptoms: dizziness, blurred vision, splitting headache, nausea, vomiting, depression, cold limbs, slippery-greasy tongue coating, bowstring-slippery pulse
Primary acupoints:
- Zhongwan (CV12)
- Fenglong (ST40)
- Touwei (ST8)
- Taiyang (MHN9)
- Secondary acupoints
- Baihui (GV20)
- Yinlingquan (SP9)
Wind-fire
Symptoms: fever, aversion to wind, inflamed eyes, restless sleep, nervousness, irritability, headache with dizziness, tinnitus, bitter taste in the mouth, red tongue with yellow coating, bowstring-rapid pulse
Primary acupoints:
- Fengchi (GB20)
- Hegu (LI4)
- Dadun (LV1)
- Xingjian (LV2)
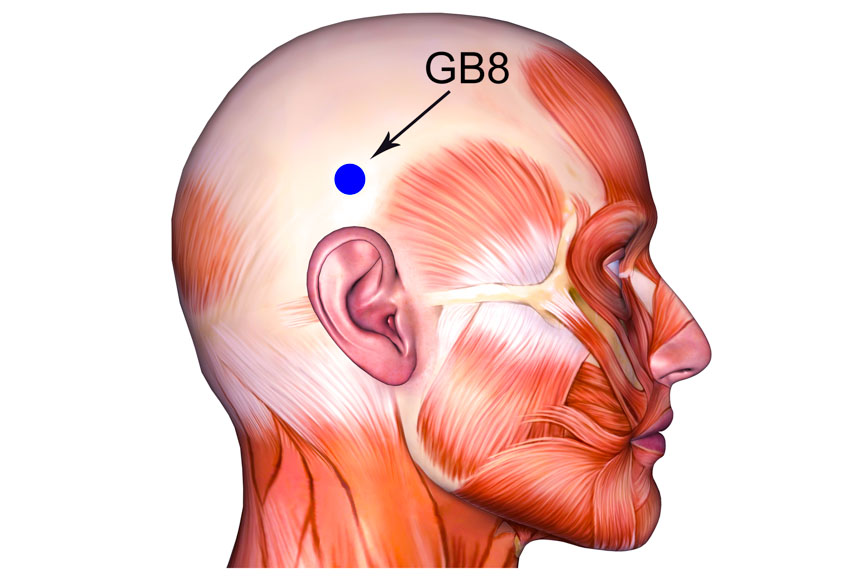
For temporal headache, add:
- Xiaxi (GB43)
- Shuaigu (GB8)
For vertex pain, add:
- Tongtian (BL7)
- Baihui (GV20)
All acupuncture treatments lasted for 30 minutes in both groups, with two weeks making up one course.
Results
Outcome measures for the study included the MPQ (McGill Pain Questionnaire), which was comprised of a PPI (Present Pain Index) and PRI (Pain Rating Index). In addition, a VAS (visual analog scale) was utilized and the total clinical effective rates calculated for both groups.
Mean pre-treatment PPI scores were 1.57 in the THP control group and 1.69 in the acupuncture group. After one course of treatment, these scores fell to 1.21 and 1.01 respectively. Mean pre-treatment PRI scores were 2.59 in the THP control group and 2.69 in the acupuncture group. After treatment, these scores fell to 1.52 and 1.24 respectively. Mean pre-treatment VAS scores were 5.12 in the THP control group and 4.69 in the acupuncture group. After treatment, these scores fell to 2.39 and 2.01 respectively.
The total clinical effective rates were calculated as follows. Patients experiencing complete resolution of headaches and other symptoms and whose laboratory test results were normal were classified as cured. For patients experiencing a near-resolution or significant improvement of headaches and complete resolution of other symptoms, whose test results were normal, and whose TCM syndrome scores reduced by ≥70%, the treatment was classified as markedly effective.
For patients experiencing a reduction in headache severity, frequency, and duration, an improvement in other symptoms and test results, and whose TCM syndrome scores reduced by ≥30%, the treatment was classified as effective. For patients experiencing no change or worsening of symptoms and test results, and whose TCM syndrome scores reduced by <30%, the treatment was classified as ineffective.
In the THP control group, there were 11 cured, 31 markedly effective, 29 effective, and 8 ineffective cases, yielding a total effective rate of 89.87%. In the acupuncture group, there were 24 cured, 46 markedly effective, 26 effective, and just 2 ineffective cases, yielding a total effective rate of 97.96%. The difference in effective rates between the two groups was of statistical significance (p<0.05). The results of this study indicate that TCM acupuncture provides significant relief from headaches.
Reference:
1. Shao Chenxu, Zhang Lide (2019) “Clinical study on acupuncture and moxibustion in treating headache” Clinical Journal of Chinese Medicine Vol.11 (15) pp. 84-86.


