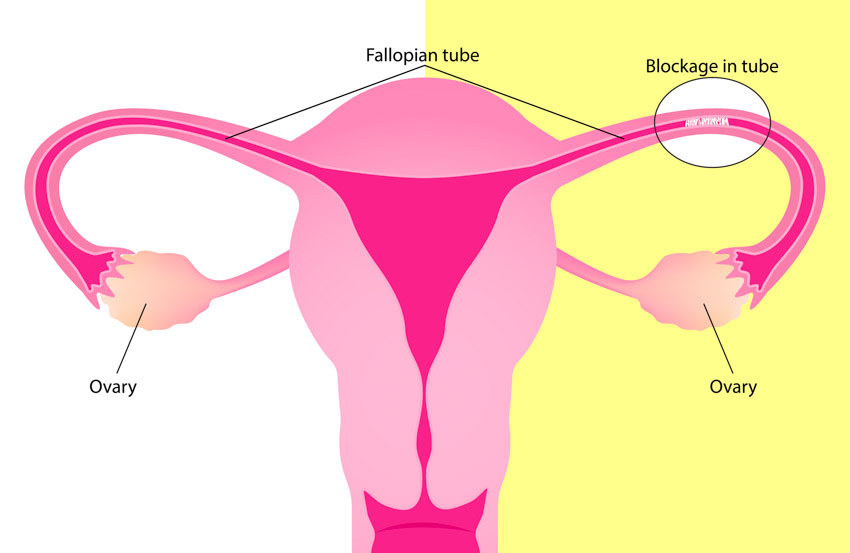
Acupuncture improves fallopian tube patency and increases pregnancy rates. A combination of warm needle acupuncture and Chinese herbal medicine improves tubal patency and increases pregnancy rates in women with fallopian tube obstruction. These are the findings of a study conducted at the Obstetrics and Gynecology Department of Tongchuan Chinese Medicine Hospital (Shaanxi, China). [1]
The study compared two groups. One received warm needle acupuncture and the herbal formula Tong Guan Tang. The other received Tong Guan Tang monotherapy. The sample size was 88 women with obstructed fallopian tubes. The total effective rate in the acupuncture plus herbs group was 93% compared with 70% in the herbal medicine monotherapy control group. A total of 39% in the acupuncture group became pregnant within 12 months of treatment, compared with 14% in the herb monotherapy control group. The study notes that acupuncture plus herbs is a safe and effective treatment for blocked fallopian tubes and is worthy of clinical promotion when applied in controlled clinical environments and only with treatment applied by licensed acupuncturists.
A total of 88 women were recruited for the study and were randomly assigned to the control group or the acupuncture group. The control group was comprised of 44 women, ages 22–37 (mean age 32 years). The women had been unsuccessfully trying to conceive for 1.5–8 years (mean 3.7 years) and there were 18 cases of primary infertility and 26 cases of secondary infertility. Of the 88 fallopian tubes in the control group, 46 were fully obstructed and 42 partially obstructed. The acupuncture group was comprised of 44 women, ages 23–38 (mean age 32.1 years). The women had been unsuccessfully trying to conceive for 2–7 years (mean 3.8 years) and there were 16 cases of primary infertility and 28 cases of secondary infertility. Of the 88 fallopian tubes in the acupuncture group, 43 were fully obstructed and 45 were partially obstructed. There were no statistically significant differences in baseline characteristics between the two groups at the outset of the investigation (p>0.05).
Acupuncture and Herbs
Both groups were treated with Tong Guan Tang, which was comprised of the following herbs:
- Huang Qi 20g
- Yi Mu Cao 20g
- Gui Zhi 15g
- Tao Ren 15g
- San Leng 15g
- Dang Gui 15g
- Chi Shao 15g
- Bai Jiang Cao 15g
- Hong Hua 12g
- Dan Pi 12g
- E Zhu 12g
- Chuan Xiong 12g
- Fu Ling 12g
- Lu Lu Tong 9g
- Gan Cao 6g
The herbs were decocted in water and taken daily while warm, split into two doses for morning and evening. The formula was introduced 3 days after the last day of the menstrual period and stopped during menstruation. A course of treatment was comprised of one menstrual cycle. After each course, a pregnancy test was administered and treatment was ceased if it was positive. If the test was negative, treatment continued for up to a total of 3 cycles. In addition to this, patients assigned to the acupuncture group received treatment at the following acupoints:
- Zigong (MCA18)
- Zhongji (CV3)
- Qihai (CV6)
- Hegu (LI4)
- Sanyinjiao (SP6)
- Taixi (KD3)
Following standard disinfection, disposable, sterile needles were inserted and manipulated by rotation, using a balanced reinforcing-reducing technique. Once in situ, a piece of moxa roll was attached to the needle handles and ignited. The needles were removed once the moxibustion completed and the needles cooled. Treatment was administered for 5 consecutive days, followed by a 2-day rest. Treatment was stopped during menstruation and each menstrual cycle made up one course of care. A pregnancy test was administered at the end of each course to determine whether treatment would cease or continue.
Results
Outcome measures for the study included ovarian artery RI (resistance index) and PI (pulsatility index) as measured by abdominal color doppler ultrasound, complete blood viscosity (high shear), fibrinogen levels, and pregnancy rates after 6 months and 1 year. The total effective rates were also calculated for each group according to overall tubal patency.
Mean pre-treatment RI was 0.56 in the control group and 0.57 in the acupuncture group. Following treatment, it fell to 0.55 and 0.51 respectively. Mean pre-treatment PI was 2.95 in the control group and 2.96 in the acupuncture group. Following treatment, it fell to 2.89 and 2.48 respectively. Significantly greater improvements in both measures were observed in the acupuncture group (p<0.05).
Mean pre-treatment blood viscosity was 5.8 mPa-s in both the control group and the acupuncture group. Following treatment, it fell to 5.5 mPa-s in the control group and 4.2 mPa-s in the acupuncture group. Mean pre-treatment fibrinogen was 4.4 g/L in both groups. Following treatment, it fell to 4.2 g/L in the control group and 3.0 g/L in the acupuncture group. Significantly greater improvements were observed in the acupuncture group (p<0.05), indicating a possible additive or synergistic effect of combined therapy.
At the 6-month follow up, 4 women in the control group and 13 in the acupuncture group had become pregnant. At the 12-month follow up, a further 2 women in the control group and 4 women in the acupuncture group had become pregnant. The overall pregnancy rates after 1 year were 14% and 39% respectively (p<0.05).
The total effective rates were calculated for each group. Each case was classified as either recovered, improved, or ineffective, according to their tubal patency as assessed by radiography. In the control group, there were 15 recovered, 16 improved, and 13 ineffective cases, giving a total effective rate of 70%. In the acupuncture group, there were 32 recovered, 9 improved, and 3 ineffective cases, yielding a total effective rate of 93%. The difference in effective rates between the two groups was statistically significant (p<0.05).
The results of this study suggest that Chinese herbal medicine improves tubal patency and pregnancy rates, but its effects are greatly enhanced by the addition of warm needle acupuncture. No adverse reactions were reported in either group, indicating that these treatments are safe and well tolerated when applied by licensed acupuncturists in controlled clinical settings.
Blocked fallopian tubes may be caused by chronic pelvic inflammatory disease. To learn how to treat this disorder, visit the following courses. The first is PID and Chinese Medicine, Part 1, which is an ebook acupuncture continuing education course. The second is Pelvic Inflammatory Disease Essentials, which is a video-based acupuncture continuing education course.
Reference:
Xiao Jinhuan (2019), “Clinical observation on treatment of infertility due to fallopian tube blockage with traditional Chinese medicine Tong Guan Tang and warm acupuncture,” Shanxi Medical Journal Vol. 48 (16) pp. 1991, 1992.


