
Acupuncture outperforms drug therapy for the treatment of insulin resistant polycystic ovary syndrome (PCOS). Shanghai Tianshan Hospital of Traditional Chinese Medicine researchers compared the efficaciousness of acupuncture with metformin hydrochloride drug therapy for the treatment of insulin resistant PCOS. Metformin hydrochloride achieved a 60.0% total effective rate and acupuncture achieved a 67.7% total effective rate. Acupuncture outperformed drug therapy for the improvement of lipid metabolism, insulin resistance, and regulation of testosterone levels. In addition, the adverse effect rate was significantly lower in the acupuncture group. [1]
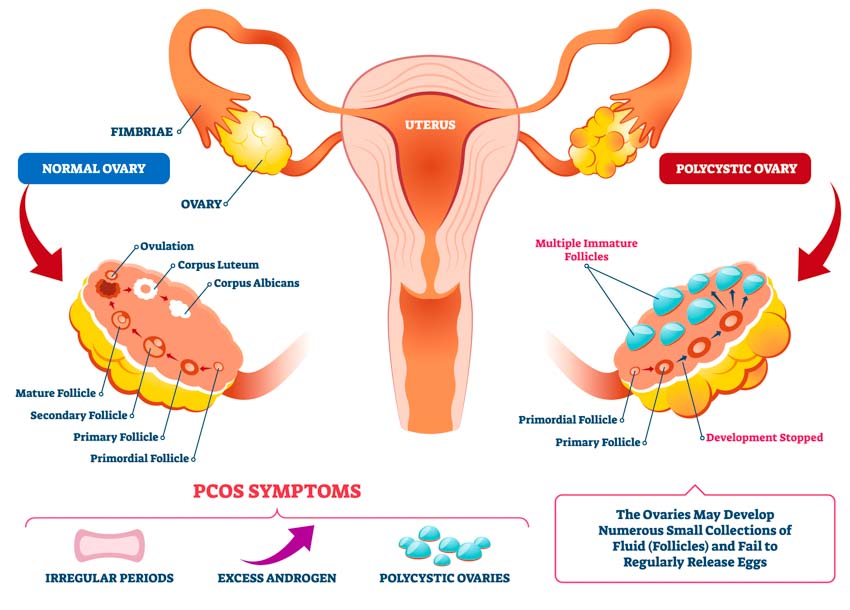
PCOS is a systemic metabolic disorder with insulin resistance and hyperandrogenism as the core pathophysiological changes. It is reported that the prevalence of PCOS is 6% to 15% in women of childbearing age. [2] One purpose of PCOS treatment is to treat and prevent metabolic complications by improving insulin resistance. Metformin is an insulin sensitizer used for the treatment of PCOS. While effective, the downside is that it can cause adverse effects including diarrhea, nausea, bloating, fatigue, indigestion, abdominal discomfort, and headaches.
Shanghai Tianshan Hospital Research
Researchers (Yu et al.) used the following study design. The study consisted of 70 patients at the acupuncture department of Shanghai Tianshan Hospital of Traditional Chinese Medicine and Shanghai Jiading District Hospital of Traditional Chinese Medicine. All patients were diagnosed with insulin resistant PCOS. They were randomly divided into an electroacupuncture treatment group and a drug control group, with 36 and 34 patients in each group respectively.
Both groups were equivalent in all relevant demographics at the beginning of the study prior to treatment. For the control group, the mean age was 31 years and the mean course of disease was 2.4 years. For the treatment group, the mean age was 30 years and the mean course of disease was 2.6 years. The inclusion criteria were as follows:
- Met the relevant diagnostic criteria for PCOS and insulin resistant.
- The TCM diagnostic pattern was phlegm dampness due to kidney deficiency
- Between 18–30 years of age
- Did not received any PCOS treatments outside the study
- Informed consent was signed for each subject.
Drug and Acupuncture Treatment
For the drug control group, patients received 500 mg doses of metformin hydrochloride tablets, twice a day, one menstrual cycle or 4 weeks as one treatment course, for a total of 3 treatment courses. The treatment was discontinued if the patients became pregnant or the fasting blood glucose was <3.6 mmol/L. Two different sets of primary acupoints were chosen for the treatment group in this study, alternating between the first and second set each day:
Set 1
- SP9 (Yinlingquan)
- CV12 (Zhongwan)
- SP6 (Sanyinjiao)
- EX-CA1 (Zigong)
- ST36 (Zusanli)
- KI3 (Taixi)
- CV4 (Guanyuan)
- ST25 (Tianshu)
- GB26 (Daimai)
- SP3 (Taibai)
- CV6 (Qihai)
- ST40 (Fenglong)
Set 2
- SP8 (Diji)
- BL22 (Sanjiaoshu)
- KI10 (Yingu)
- BL20 (Pishu)
- BL18 (Ganshu)
- EX-B3 (Yishu, Weiguanxiashu)
- BL23 (Shenshu)
- SP4 (Gongsun)
- BL32 (Ciliao)
The secondary acupoints selected for the study were the following:
- LI4 (Hegu)
- LV3 (Taichong)
Treatment commenced with patients in a supine position for the first set of acupoints or in a prone position for the second set. After disinfection of the acupoint sites, a 0.30 mm × 40–70 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. For Zigong, the needle was inserted toward the abdominal middle line at an angle of 60 degrees to the skin, reaching a depth of 30–70 mm. For Back Shu points, the needle was inserted toward the spine at an angle of 30–60 degrees, reaching a depth of 20–40 mm. The rest of the acupoints were inserted perpendicularly. Upon arrival of a deqi sensation, the Ping Bu Ping Xie (mild tonifying and attenuating) manipulation technique was applied to each needle every 10 minutes during a 30-minute needle retention time.
After needle insertion, a G6805-II electroacupuncture device was connected to the needles. For the first set of primary acupoints, a pair of positive and negative electrodes were attached to the following acupoint combinations respectively: Daimai and Zigong (ipsilateral), Zhongwan and Tianshu (left), Qihai and Tianshu (right). For the second set, a pair of positive and negative electrodes were attached to the following acupoint combinations: Yishu and Pishu (ipsilateral), Ciliao and Shenshu (ipsilateral). 2 Hz continuous wave stimulation was applied with an intensity level set to patient tolerance levels during the 30-minute needle retention time. The electroacupuncture treatment was applied 3 times per day (every 1–2 days), one period cycle or 4 weeks as one treatment course, for a total of 3 treatment courses.
Scoring
Multiple biochemical indicators were measured before treatment and 3 months after treatment. First, the lipid metabolism was determined by measuring triacylglycerol (TG), total cholesterol (TC), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) levels. Second, homeostasis model assessment-insulin resistance index (HOMA-IR) was calculated. Third, serum testosterone (T) levels were compared before and after treatment. Fourth, the treatment efficacy for each patient was categorized into 1 of 4 tiers:
- Recovery: Pregnancy during treatment or within 3 months after treatment. Normal menstrual cycle, volume, color, and other characteristics. Normal serum testosterone levels. HOMA-IR <2.69. Disappearance of clinical symptoms.
- Significantly effective: Appearance of menstrual period during treatment or within 3 months after treatment. Significant improvement of menstrual cycle, volume, color and other characteristics. Significant improvement of serum testosterone levels. HOMA-IR <2.69. significant alleviation of clinical symptoms.
- Effective: Improvement of clinical symptoms. Improvement of menstrual cycle, volume, color and other characteristics. Improvement of serum testosterone levels.
- Ineffective: No improvement of clinical symptoms, menstrual cycle, volume, color and other characteristics, as well as serum testosterone levels.
Results
After treatment, the levels of serum T, HOMA-IR, LDL, TG, and TC decreased significantly in the two groups (p<0.01, p<0.05), and HDL increased significantly (p<0.01); the level of TC in the electroacupuncture group after treatment was significantly lower than that in the medication group (p<0.05). In addition, a total of 10 patients in the medication group reported different degrees of diarrhea, bloating, and other adverse reactions, of which 4 patients requested to discontinue treatment. Only 4 patients in the electroacupuncture group had mild adverse reactions such as subcutaneous hematoma, which didn’t require discontinuation of treatment. The researchers conclude that acupuncture is safer and more effective for the treatment of insulin resistant PCOS than metformin hydrochloride.
References:
[1] Yu LQ, Cao LY, Xie J, et al. Efficacy and mechanism of electroacupuncture on insulin resistant polycystic ovary syndrome[J]. Chinese Acupuncture and Moxibustion, 2020,04:379-383.
[2] Klimczak D, Szlendak-Sauer K, Radowicki S. Depression in relation to biochemical parameters and age in women with polycystic ovary syndrome[J]. Eur J Obstet Gynecol Reprod Biol, 2015, 184: 43-47.


