Acupuncture and the external application of herbal medicine provide facial paralysis relief. Chenzhou Hospital of Traditional Chinese Medicine researchers demonstrate that acupuncture, combined with herbal steaming and washing, provides effective relief for patients with peripheral facial nerve palsy (FNP). [1]
The study compared two protocols. One group received acupuncture plus herbal steaming and washing. Another study group received acupuncture plus internal herbal medicine. Both groups demonstrated significant improvements. The acupuncture plus external application of herbs group had a 96% total effective rate. The acupuncture plus internal herbs group had an 84% total effective rate. Results were based on symptom scores and HB (House Brackmann) facial function scores.
Peripheral facial nerve palsy (FNP) is often caused by viral infections, post-surgical complications, trauma, diabetes, bacterial infections, tumors, adverse effects from medications, and immune system disorders. Bell’s Palsy is one type of peripheral facial nerve paralysis and is classified as an idiopathic paralysis due to inflammation of the seventh cranial nerve. In this study, 100 FNP patients (in the acute or recovery phase) were recruited. They were assigned by the random number table method to the acupuncture plus external herbs group or the acupuncture plus internal herbs group.
The acupuncture plus external herbs group was comprised of 25 male and 25 female patients, ages 21–60 years (mean age 40.32 years). The acupuncture plus internal herbs group was comprised of 26 male and 24 female patients, ages 20–61 (mean age 41.54 years). There were no statistically significant differences in baseline characteristics between the two groups upon admission to the investigation.
Acupuncture And Herbs
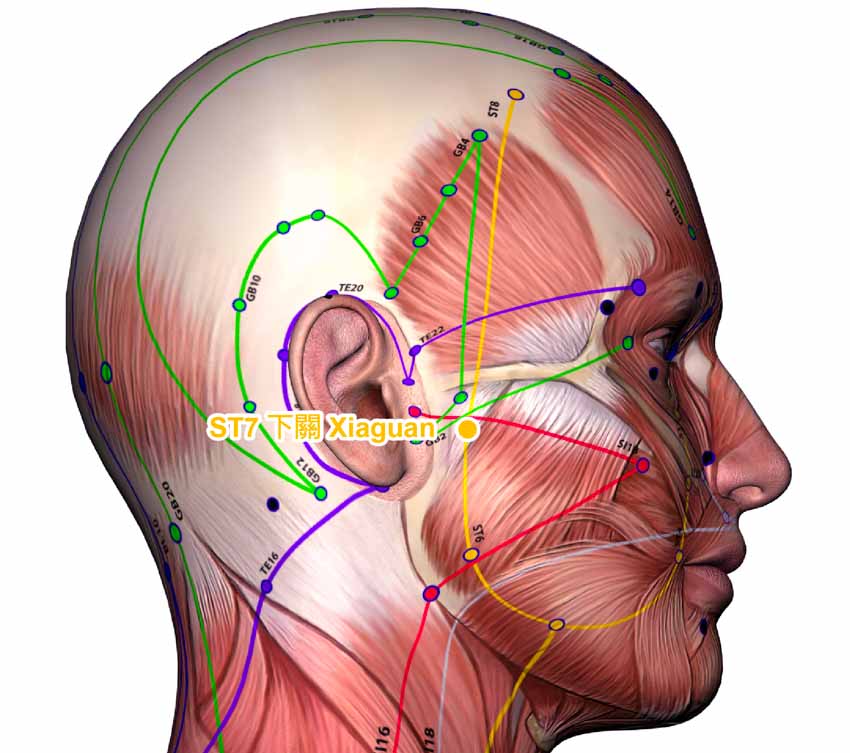
The participants in both groups received the same acupuncture treatment. During the acute phase, acupuncture was administered to a selection of points on the affected channels, including the following:
- Fengchi (GB20)
- Taichong (LV3)
- Baihui (GV20)
- Hegu (LI4)
- Fengfu (GV16)
After one week of treatment, the following acupoints were added:
- Shenting (GV24)
- Yifeng (TB17)
- Juliao (ST3)
- Taiyang (MHN9)
- Xiaguan (ST7)
Sterile, 0.30 × 40 mm needles were selected and inserted to a depth of 0.8–1 cun. The needles were manually stimulated using a balanced reinforcing-reducing method and were retained for 30 minutes. Participants in the acupuncture plus internal herbs group were prescribed herbal medicine according to their presenting TCM syndrome:
- Patients with wind-cold attacking the network vessels were prescribed Ma Huang Fu Zi Xi Xin Tang Jia Jian.
- Patients with wind-heat attacking the network vessels were prescribed Da Qin Jiao Tang Jia Jian.
- Patients with wind-phlegm obstruction were prescribed Qian Zheng San Jia Jian.
- Patients with qi deficiency and blood stasis were prescribed Bu Yang Huan Wu Tang Jia Jian.
Participants in the acupuncture plus external herbs group were treated with herbal steaming and washing. The formula was comprised of the following herbs:
- Jiang Can 10g
- Chi Shao 10g
- Bai Zhi 10g
- Yun Mu Xiang 10g
- Fang Feng 10g
- Wu Yao 10g
- Chai Hu 10g
- Di Long 10g
- Tou Gu Cao 10g
- Wu Gong – 1 piece
- Dan Shen 16g
- Bai Shao 16g
- Bai Fu Zi 12g
- Dang Gui 12g
- Chuan Xiong 12g
- Ju Hua 6g
- Huang Qi 20g
- Wu Shao She 3g
- Jing Jie 8g
The herbs were soaked in water for 20 minutes before decoction. The resulting liquid was filtered and 1800 mL was placed inside a HY2-IC medical fumigator. The liquid was maintained at 35–40 degrees Celsius (95–104 degrees Fahrenheit) and were used to steam the affected side of the patients’ faces. With the patients in a supine position, the fumigator nozzle was positioned 30–50cm away from the patients was and directed at the affected area and mastoid. The heated vapor was sprayed evenly onto the skin for a total of 30 minutes. All treatments in both groups were administered for ten continuous days, followed by a two-day rest. A total of three courses were administered.
Outcomes and Discussion
Outcome measures for the study included TCM symptom scores, HB scores, and the total clinical effective rates for each group. Mean pre-treatment TCM symptom scores were 20.87 in the acupuncture plus internal herbs group and 20.54 in the acupuncture plus external herbs group. Following treatment, scores fell to 8.64 and 4.39, respectively. Mean pre-treatment HB scores were 4.35 in the acupuncture plus internal herbs group and 4.33 in the acupuncture plus external herbs group. Following treatment, scores fell to 3.65 and 2.72, respectively. The clinical effective rates were calculated for each group according to degree of improvement in each patient’s symptoms:
- Patients with normal facial nerve function (HB Grade I) were classified as recovered.
- For patients with slight facial nerve dysfunction and synkinesis, normal symmetry and muscle tone at rest, the ability to close the eyes with minimal effort, moderate to good forehead movement, and slight mouth asymmetry (HB Grade II), the treatment was classified as markedly effective.
- For patients with an obvious but not disfiguring asymmetry between the two sides of the face, noticeable but not severe synkinesis, the ability to close the eyes with effort, slight to moderate forehead movement, and slight weakness of the mouth (HB Grade III), the treatment was classified as effective.
- For patients with noticeable facial asymmetry at rest, inability to close the eyes, no forehead movement, and only slight mouth movement (HB Grades IV–VI), the treatment was classified as ineffective.
In the acupuncture plus internal herbs group, there were 9 recovered, 21 markedly effective, 12 effective, and 8 ineffective cases, yielding a total effective rate of 84%. In the acupuncture plus external herbs group, there were 10 recovered, 28 markedly effective, 10 effective, and just 2 ineffective cases, yielding a total effective rate of 96%. The results of this study indicate that acupuncture and herbs are effective for FNP patients in the acute and recovery stages. Furthermore, the treatment can be significantly enhanced by the addition of herbal steaming and washing.
Reference:
[1] Wu Jiliang, Li Kunxiang, Zhou Yulin, Xia Pei, Zhou Jiang (2019) “Clinical Study on Acupuncture and Moxibustion Combined with Fumigation and Washing of Traditional Chinese Medicine in Treatment of Peripheral Facial Paralysis in Acute and Convalescent Stages” Journal of Practical Traditional Chinese Internal Medicine Vol.33 (8) pp.44-45.


