Acupuncture reduces the frequency of migraine headache attacks. Hospital and university researchers tested a specific set of acupuncture points for clinical efficacy. A team of 14 licensed acupuncturists (with at least 5 years of professional experience each) administered 20 acupuncture treatments in a randomized controlled trial. Each acupuncture treatment lasted for 30 minutes. Patients received acupuncture treatments every other day for the first 10 sessions, followed by a 9 day break, and then received another 10 sessions of acupuncture every other day.
The total sample size was 147 patients. Three groups were compared: true manual acupuncture, placebo needle sham acupuncture, usual care monotherapy. True manual acupuncture significantly outperformed both sham acupuncture and usual care monotherapy. Patients receiving true acupuncture had fewer migraine attacks, with significant positive patient outcomes (fewer days with migraines per month). [1]
An important trend emerged. Patients having received acupuncture had increasing rates of improvement over time. Improvements were significant during the first 4 weeks of acupuncture treatment. The trend line continued to show fewer and fewer migraine attacks at each consecutive data point (weeks: 1–20, 13–16, 17–20). The 20 week follow-up assessments reveal that acupuncture produces lasting beneficial effects.
The study was a single blinded, randomized three arm clinical trial of human volunteers. A neurologist was responsible for diagnosing participants (migraines without aura) prior to randomization. Exclusion criteria included other types of headaches.
All patients received basic usual care, which included teaching patients about lifestyle self-management. A rescue remedy was allowed for patients (diclofenac sodium tablets) for severe pain. That is the only treatment provided during the study for the usual care group; however, the study team did allow usual care group patients to receive acupuncture after waiting 24 weeks after the clinical trial.
The sham acupuncture group received Streitberger placebo needles, which are blunt tip devices that do not penetrate the skin and retract into the shaft when simulating insertion. All members of the true acupuncture group received acupuncture at the following acupoints:
- LI4 (Hegu)
- LV3 (Taichong)
- Taiyang (Extra MH9)
- GB20 (Fengchi)
- GB8 (Shuaigu)
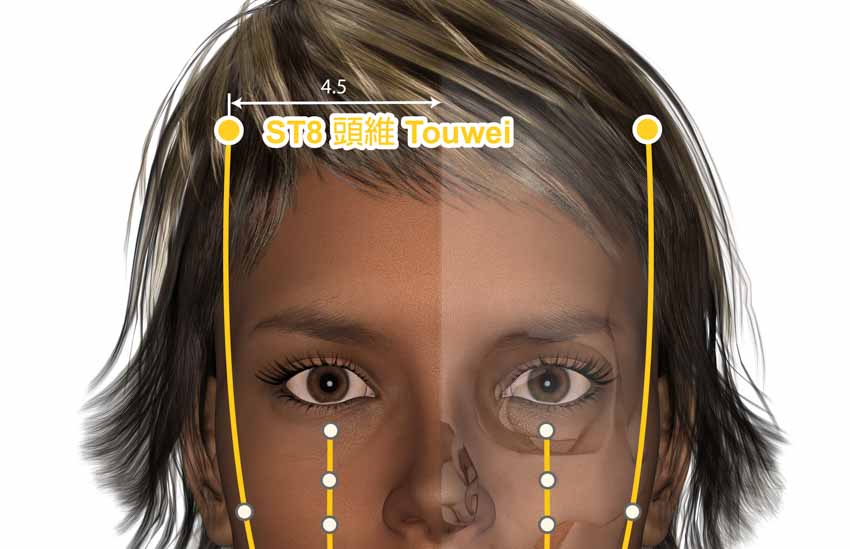
Using a semi-protocolized design, the following modifications were allowed per individual patient diagnostics. For yangming channel headaches, ST8 (Touwei) was added. For taiyang channel headaches, BL10 (Tianzhu) was added. For jueyin channel headaches, DU20 (Baihui) was added.
Acupuncture needles were 0.30 × 30 mm and manual stimulation to achieve deqi at each acupoint lasted for 10 seconds. Manual stimulation was repeated a total of 4 times at 10 minute intervals. The researchers concluded, “Twenty sessions of manual acupuncture was superior to sham acupuncture and usual care for the prophylaxis of episodic migraine without aura.” [2]
The findings are consistent with an outside independent investigation. Harvard Medical School, Georgetown University, University of Arizona, Creighton University, and Louisiana State University researchers conclude that acupuncture reduces the frequency, intensity, and duration of migraine attacks. [3] The researchers indicate that patients receiving acupuncture are also less prone to secondary anxiety attacks and depression.
In another investigation, Harvard Medical School, Xidian University, and Capital Medical University researchers find acupuncture effective for the reduction of migraine attack frequency. [4] Patients received 3 acupuncture treatments per week for 4 weeks. Each acupuncture treatment was 30 minutes. The acupuncture points used were the following:
- GV20 (Baihui)
- GV24 (Shenting)
- GB13 (Benshen)
- GB8 (Shuaigu)
- GB20 (Fengchi)
The researchers reveal that a patient’s pre-treatment brain structure is predictive of the success rate achieved by acupuncture. Using MRIs and machine learning, specific patterns in brain gray matter prior to treatment were correlated with improved response rates to the acupuncture point prescription used in the investigation. The researchers indicate that MRI findings may contribute to determining patient outcomes prior to treatment.
References:
1. Xu, Shabei, Lingling Yu, Xiang Luo, Minghuan Wang, Guohua Chen, Qing Zhang, Wenhua Liu et al. "Manual acupuncture versus sham acupuncture and usual care for prophylaxis of episodic migraine without aura: multicentre, randomised clinical trial." bmj 368 (2020).
2. ibid.
3. Urits, Ivan, Megha Patel, Mary Elizabeth Putz, Nikolas R. Monteferrante, Diep Nguyen, Daniel An, Elyse M. Cornett, Jamal Hasoon, Alan D. Kaye, and Omar Viswanath. "Acupuncture and Its Role in the Treatment of Migraine Headaches." Neurology and Therapy (2020): 1-20. Author Affiliations:
Department of Anesthesia, Critical Care, and Pain Medicine, Beth Israel Deaconess Medical Center— Harvard Medical School, Boston, Massachusetts.
Department of Anesthesiology, University of Arizona College of Medicine–Phoenix, Phoenix, Arizona.
Department of Anesthesiology, Creighton University School of Medicine, Omaha, Nebraska.
Georgetown University School of Medicine, Washington, DC.
Department of Anesthesiology, Louisiana State University Health Shreveport, Shreveport, Louisiana.
Valley Pain Consultants–Envision Physician Services, Phoenix, Arizona.
4. Yang, X.J., Liu, L., Xu, Z.L., Zhang, Y.J., Liu, D.P., Fishers, M., Zhang, L., Sun, J.B., Liu, P., Zeng, X. and Wang, L.P., 2020. Baseline Brain Gray Matter Volume as a Predictor of Acupuncture Outcome in Treating Migraine. Frontiers in Neurology, 11, p.111.


