Acupuncture increases the total effective rate of drug therapy for the relief of obstructive sleep apnea-hypopnea syndrome (OSAHS). Shanghai Jiaotong University School of Medicine researchers combined acupuncture with drug therapy (montelukast plus mometasone). Patients receiving only medications had a 60.0% total effective rate. The addition of acupuncture increased the effective rate to 80.0%. [1] The results were measured with the apnea hypopnea index (AHI), minimum nocturnal arterial oxygen saturation scores (SaO2), and attention impairment indicators at the completion of all medical treatments.
Researchers (Yu et al.) used the following study design. A total of 60 pediatric patients were treated and evaluated. The patients were diagnosed with mild to moderate OSAHS. They were randomly divided into an acupuncture treatment group and a control group, with 30 patients in each group. For the control group patients, montelukast granules and mometasone nasal spray were administered. The treatment group received acupuncture in addition to the identical drug treatments administered to the drug control group.
The statistical breakdown for each randomized group was as follows. For both groups, there were 14 males and 16 females. The youngest age was three years; the eldest was six years of age. The shortest course of disease was three months, and the longest was 14 months. There were no significant statistical differences in gender, age, and course of disease relevant to patient outcome measures for patients initially admitted to the study.
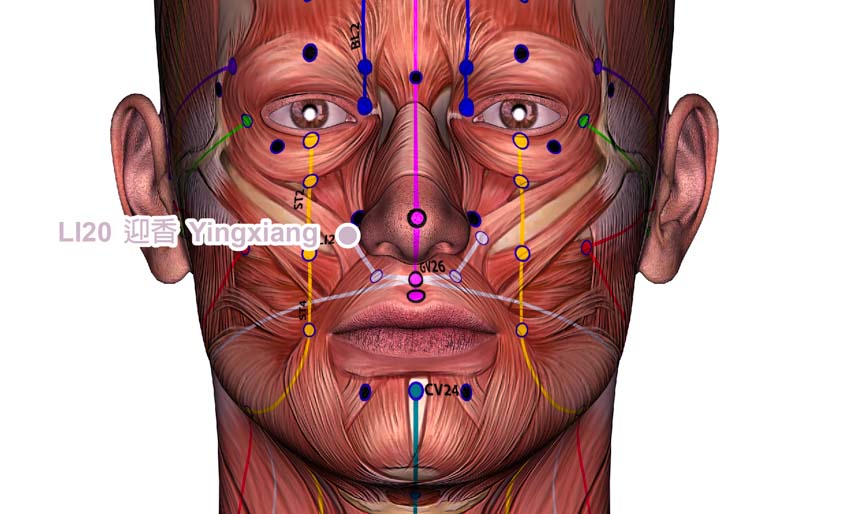
All patients received montelukast granules and mometasone nasal spray (4 mg montelukast granules, 1 spray of mometasone into each nostril each day). The drug treatment lasted for three months. Montelukast (brand name Singulair) is an oral leukotriene receptor antagonist. Mometasone is a steroid. Both medicines are used to address airway narrowing. The primary acupoints used for the treatment group included the following:
- LI20 (Yingxiang)
- EX-HN3 (Yintang)
- GV23 (Shangxing)
- LI4 (Hegu)
- ST9 (Renying)
- CV23 (Lianquan)
Secondary acupuncture points were added based on diagnostic considerations. For patients with lung qi deficiency, the following acupoint was added: BL13 (Feishu). For patients with spleen qi deficiency, the following acupoints were added: BL20 (Pishu), ST36 (Zusanli). Acupuncture treatments commenced with patients in a sitting position. After disinfection of the acupoint sites, a 0.35 mm x 13–25 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed.
For Yingxiang, the needle was inserted towards the location of Bitong (EX-HN18) with the lifting technique, up to a depth of 0.5 cun. For Yintang, the needle was inserted toward the nasal root and was applied with the lifting technique to achieve a deqi sensation towards the nasal tip. For Shangxing, the needle was inserted towards the nasal tip for a length of of 1 cun, transversely.
For Hegu, the needle was inserted obliquely and proximally to a depth of 1–1.5 cun. For Renying and Lianquan, needles were inserted at an angle of 90–180 degrees and were twisted at a frequency of 200 times/min for 30 seconds. No needle retention was needed for these two points. For Feishu, Pishu, and Zusanli, the needles were inserted perpendicularly for a depth of 0.5–1 cun. Except for Renying and Lianquan, the needles were retained for 30 min. The treatment was performed 3 times a week, for a total of 3 months.
Patients were evaluated before and after the treatment course. First, AHI and the minimum nocturnal SaO2 levels were measured to determine OSAHS severity. Second, the full-scale attention quotient (FSAQ) and full-scale response control quotient (FSCQ) were calculated to quantify attention impairment. Third, the treatment efficacy for each patient was categorized into 1 of 4 tiers based on AHI and SaO2 levels:
- Recovery: Absence of symptoms. No apnea or hypopnea. The minimum SaO2 > 90%.
- Significantly effective: Significant absence of symptoms. AHI ≥ 1 and ≤ 5 times/h. The minimum SaO2 between 85 – 90%.
- Effective: Symptoms showed improvement. AHI ≥ 5 and ≤ 15 times/h. The minimum SaO2 between 80 – 94%.
- Not effective: Symptoms showed no visible improvement.
The total effective rate was 80.0% in the acupuncture treatment group and 60.0% in the drug monotherapy control group with a statistically significant difference between the two groups. There were statistically significant post-treatment differences in AHI, SaO2 scores, and attention impairment indicators between the two groups.
The results indicate that using acupuncture in an integrative treatment protocol significantly increases the effective rate. Yu et al. conclude that acupuncture is an effective treatment for the relief of mild to moderate pediatric OSAHS and significantly improves outcomes for drug therapy patients.
Reference:
[1] Yu PB, Ding LF, Chen J. Observations on the Efficacy of Combined Acupuncture and Medicine for Mild to Moderate Obstructive Sleep Apnea-Hypopnea Syndrome [J]. Shanghai Journal of Acupuncture and Moxibustion, 2021, 40(02):163-167.


