Acupuncture controls inflammation. Recent investigations demonstrate that acupuncture has powerful anti-inflammatory effects. This applies to pain relief, immune system responses, and general inflammation throughout the body.
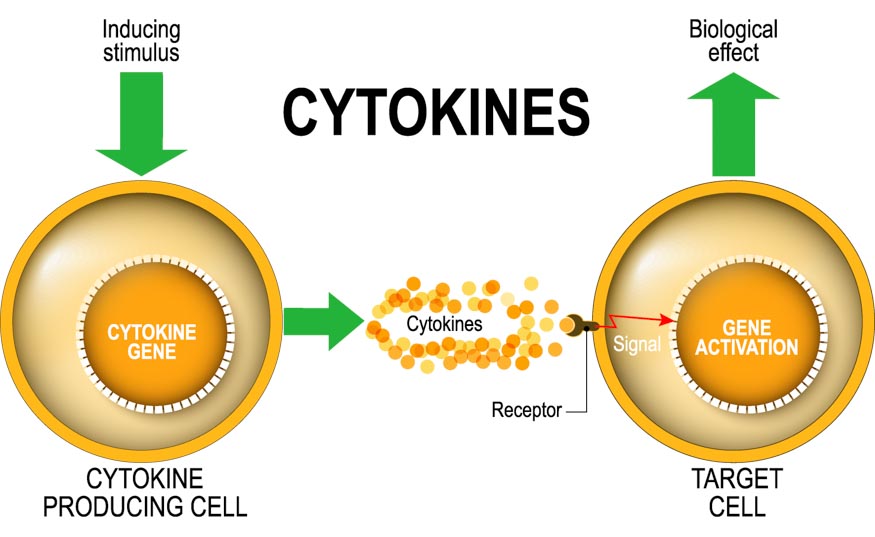
Harvard Medical School neuroscientists determined that acupuncture reduces bacterial infection related inflammation. [1] The neuroscientists demonstrated that acupuncture reduces the intensity of pro-inflammatory cytokine storms. Their laboratory research shows that acupuncture increases survival rates and prevents disease progression.
The Harvard Medical School neuroscientists determined that low intensity electroacupuncture stimulation at acupoint ST36 (Zusanli) activates anti-inflammatory responses after exposure to bacterial endotoxins. In addition, high intensity electroacupuncture stimulation at ST25 (Tianshu) suppresses splenic inflammation if applied prior to endotoxin exposure.
Acupuncture is effective for reducing inflammation in patients with rheumatoid arthritis. China Medical University and Tri-Service General Hospital researchers conducted a meta-analysis. They determined that acupuncture beneficially regulates the erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and rheumatoid factor (RF) levels, interleukins, nuclear factor kappa B (NF-𝜅 B), and tumor necrosis factor alpha (TNF-𝛼). [2]
In another study, Dong et al. used laboratory conditions to test the efficacy of electroacupuncture at acupoints ST36 (Zusanli) and BL60 (Kunlun). The researchers note that the “toll-like receptor (TLR) signaling pathway contributed to the development and progression of RA [rheumatoid arthritis] and acupuncture could reduce the expression of TLR4, thus leading to anti-inflammation.” [3]
Chinese herbal medicine also produces significant anti-inflammatory effects. In an investigation of COVID-19 patients with pneumonia, researchers conclude that the addition of Chinese medicine to usual care improves clinical efficacy. The researchers note that Chinese medicine “significantly increased [the] viral nucleic acid negative conversion rate.” They note that Chinese medicine “prominently reduced pulmonary inflammation,” “improved host immune function,” and Chinese medicine “exhibited superior performance” for improving the “clinical effective rate, viral nucleic acid negative conversion rate, remission rate of pulmonary inflammation, and biochemical markers.” [4]
The combination of acupuncture and herbal medicine has also been shown to reduce inflammation. Shaoxing Seventh People’s Hospital researchers conclude that a modified version of the herbal formula Chai Hu Shu Gan San plus acupuncture is effective for the alleviation of depression. Based on the Hamilton Depression Rating Scale, serum cytokine, and neurotransmitter levels, the total effective rate was 100% for patients receiving acupuncture plus Chinese herbal medicine. Patients receiving acupuncture monotherapy had an 85% total effective rate and patients receiving Chinese herbal medicine monotherapy had an 87.5% total effective rate. [5]
In group A (herbal monotherapy), there were 15 clearly effective, 20 effective, and 5 ineffective cases, producing a total effective rate of 87.5%. In group B (acupuncture monotherapy), there were 15 clearly effective, 19 effective, and 6 ineffective cases, producing a total effective rate of 85%. In group C (acupuncture combined with Chinese herbal medicine), there were 19 clearly effective, 21 effective, and no ineffective cases, producing a total effective rate of 100%.
Serum cytokine levels measured by the researchers included IL-6, TNF-α, and IL-1β. These pro-inflammatory cytokines are correlated with central nervous system changes and are markers of depression. Group A mean pre-treatment IL-6 levels (pg/mL) were 16.63. In Group B, the mean levels were 16.72 and they were 16.59 in group C. Following treatment in groups A, B, and C, the levels reduced to 10.52, 10.35, and 6.20 respectively. The combination group (group C) demonstrated the most significant improvements. The same pattern was documented for TNF-α and IL-1β levels, with the combination group demonstrating the greatest improvements.
Increases in serum neurotransmitter levels were documented. These levels are often low in patients with depression. Serotonin (5-HT), norepinephrine (NE), and brain derived neurotrophic factor (BDNF) levels improved significantly in all three test groups. The acupuncture plus herbs combination group demonstrated the greatest improvements. A modified version of the herbal formula Chai Hu Shu Gan San was used:
- Chen Pi 6 grams
- Chai Hu 6 g
- Chuan Xiong 4.5 g
- Xiang Fu 4.5 g
- Zhi Ke 4.5 g
- Bai Shao Yao 4.5 g
- Zhi Gan Cao 1.5 g
For patients with tongue petechiae (small red or purple dots), both Dang Gui and Dan Shen were supplemented to the formula. Each herbal preparation was decocted in water and divided into two portions, taken two times daily. For patients receiving acupuncture, the following acupuncture points were applied:
- Yintang (extra point)
- Baihui (DU20)
- Sishencong (extra point)
- Shenting (DU24)
- Neiguan (P6)
- Shenmen (HT7)
- Sanyinjiao (SP6)
- Hegu (LI4)
- Taichong (LV3)
- Taiyang (extra point)
Overall, there is a distinct pattern in modern research. Acupuncture demonstrates significant anti-inflammatory capabilities. In addition, anti-inflammatory responses are enhanced with the addition of herbal medicine.
References
[1] Liu, Shenbin, Zhi-Fu Wang, Yang-Shuai Su, Russell S. Ray, Xiang-Hong Jing, Yan-Qing Wang, and Qiufu Ma. "Somatotopic Organization and Intensity Dependence in Driving Distinct NPY-Expressing Sympathetic Pathways by Electroacupuncture." Neuron (2020).
[2] Chou, Pei-Chi, and Heng-Yi Chu. "Clinical Efficacy of Acupuncture on Rheumatoid Arthritis and Associated Mechanisms: A Systemic Review." Evidence-Based Complementary and Alternative Medicine 2018 (2018).
[3] Z.-Q. Dong, J. Zhu, D.-Z. Lu, Q. Chen, and Y.-L. Xu, “Effect of Electroacupuncture in “Zusanli” and “Kunlun” Acupoints on TLR4 Signaling Pathway of Adjuvant Arthritis Rats,” American Journal ofTherapeutics, 2016.
[4] Sun, Chun-Yang, Ya-Lei Sun, and Xin-Min Li. "The role of Chinese medicine in COVID-19 pneumonia: A systematic review and meta-analysis." The American Journal of Emergency Medicine (2020).
[5] Tong Weilong, Wu Jingzhu, Zhao Guiqin, Zhao Mingyong, “Study on Effect of Modified Chaihu Shugan Powder Combined with Acupuncture in Patients with Depression and Influence for Related Indexes,” Chinese Archives of Traditional Medicine Vol. 37 (1), 227-229 (2019).


