Researchers confirm that acupuncture is effective for the treatment of Bell’s palsy. In one investigation, acupuncture plus standard drug therapy outperformed drug monotherapy. In another independent investigation, researchers found that applying low frequency electroacupuncture produces significant positive outcomes for acute Bell’s palsy patients. Let’s take a look at both investigations.
The following study demonstrates the effectiveness of integrative medicine. Acupuncture plus drug therapy (prednisone and acyclovir) outperforms drug monotherapy for Bell’s palsy treatment efficaciousness. Shanghai No. 6 People’s Hospital researchers determined that acupuncture has a 96.67% total effective rate when combined with prednisone and acyclovir treatments. As a standalone therapy, patients taking oral prednisone (a corticosteroid anti-inflammatory medicine) and acyclovir (an anti-viral drug) achieved an 81.67% total effective rate. Results were determined by analysis of the Facial Nerve Grading Stennert Index and electromyography. [1]
At HealthCMi, we feature the free news and research service along with acupuncture CEU on-demand courses and live webinars. To learn about Bell’s Palsy in an acupuncture continuing education online course, visit the following:
Bells Palsy and Chinese Medicine >
The study involved the selection of 120 patients. They were randomly divided into an acupuncture plus drug treatment group and a drug control group, with 60 patients in each group. The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 38 males and 22 females. The average age in the treatment group was 44.3 ±12.8 years. The average course of disease in the treatment group was 3.26 ±1.21 days.
The drug control group was comprised of 33 males and 27 females. The average age in the drug control group was 43.35 ±15.1 years. The average course of disease in the drug control group was 4.06 ±1.54 days. For both groups, there were no significant differences in terms of their gender, age, and course of disease prior to initiation of the investigation.
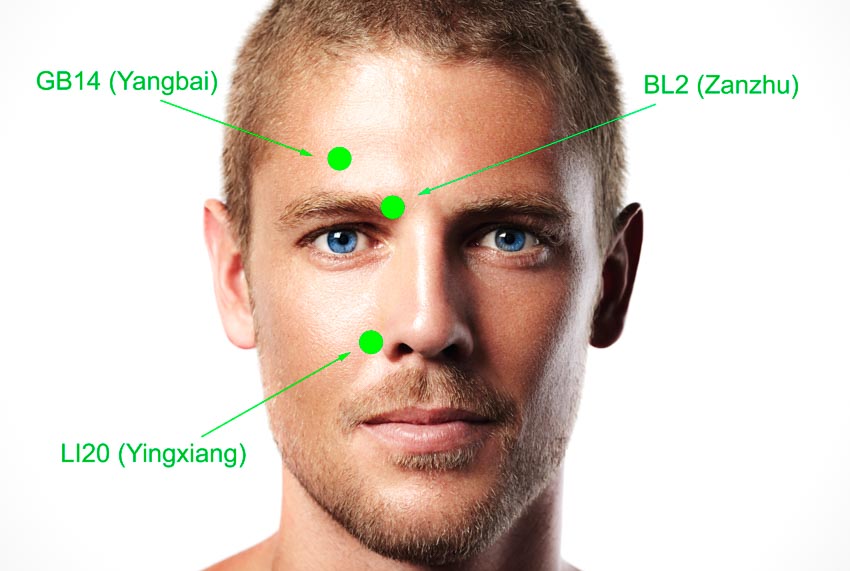
For both groups, prednisone and acyclovir tablets were orally administered. Patients received doses of prednisone tablets for 12 days (Day 1 – 3: 30 mg, Day 4 – 6: 20 mg, Day 7 – 9: 10 mg, Day 10 – 12: 5 mg). At the same time, 0.4 g of acyclovir tablets were given three times per day, for a total of nine days. The treatment group also received acupuncture treatment at the following acupoints:
- GB14 (Yangbai)
- ST6 (Jiache)
- Extra Acupoint (Qianzheng)
- ST4 (Dicang)
- TB17 (Yifeng)
Note: Extra acupoint Qianzheng (Pull Upright) is located 0.5 to 1 cun anterior to earlobe (lobulus auriculae). Indications for use include facial paralysis, deviation of the eyes and mouth, and mouth and tongue ulcers.
Additional acupoints were administered based on differential diagnostic patterns. For difficulty or weakness in raising the eyebrows, the following acupuncture points were added:
- BL2 (Cuanzhu)
- TB23 (Sizhukong)
For incomplete closure of the eyes, the following acupoint was added:
- GB1 (Tongziliao)
For shallowing or disappearance of the nasolabial folds, the following acupuncture points were added:
- LI20 (Yingxiang)
- ST2 (Sibai)
For deviation of the mouth, the following acupoint was added:
- GV26 (Renzhong)
For pain behind the ear and stiffness in the neck, the following acupoint was added:
- GB20 (Fengchi)
For numbness of the tongue and loss of taste, the following acupoint was added:
- CV23 (Lianquan)
After disinfection of the acupoint sites, 0.30 mm x 40 mm or 0.35 mm x 75 mm acupuncture needles were obliquely inserted into each acupoint. For Dicang, the needle was threaded for 2 cun. Other acupoints were inserted or threaded to a depth of 0.5 cun. Each needle was retained for 15 minutes upon insertion, without the application of any manual techniques. The acupuncture treatment was administered every two days, and a total of 10 treatments were given.
Patients receiving both acupuncture and standard drug therapy had a 96.67% total effective rate, while patients receiving only drugs had an 81.67% total effective rate. In addition, electromyography revealed that the combined treatment protocol group produced more prolonged latency and lower amplitude scores, indicating better treatment outcomes compared with the drug control group.
In a related finding, Zhao et al. conclude that electroacupuncture is effective for the treatment of Bell’s palsy. [2] The House-Brackman Scale, Sunnybrook Scale, electromyography, and MRIs were used to record the results. The acupoints used in the study were the following:
- GB14 (Yangbai, affected side)
- TB23 (Sizhukong, affected side)
- SI18 (Quanliao, affected side)
- Extra Acupoint (Qianzheng, affected side)
- LI20 (Yingxiang, affected side)
- GB20 (Fengchi, affected side)
- LI4 (Hegu, bilateral)
- LV (Taichong, bilateral)
A 0.30 mm x 25 mm needle was inserted perpendicularly into each acupoint, reaching a depth of 10–17 mm. Upon achieving a deqi sensation, the following acupoints were connected to an electroacupuncture device: Yangbai-Sikongzhu, Qianzheng-Dicang, and Quanliao-Yingxiang. A 2 Hz disperse-dense wave was applied. The needles were retained for 20 minutes.
The benefits of electroacupuncture for Bell’s palsy patients including improvements in the House-Brackman Scale and Sunnybrook Scale scores, facial nerve functions (including latency, amplitude, and amplitude ration), and MRI results. The researchers conclude that the application of low frequency electroacupuncture is effective for the treatment of acute Bell’s palsy.
References:
[1] Zhao Chang, Liu Zhidan, etc. (2018). Effects of Low Frequency Electroacupuncture on Acute Bell’s Palsy. Journal of Clinical Acupuncture and Moxibustion, (03), 8-15. doi: CNKI:SUN:ZJLC.0.2018-03-004.
[2] Zhang Junfeng, Wang Jianxiong. (2014). Acupuncture for Treating Acute Intractable Facial Paralysis: Large sample Randomized Controlled Trial. Journal of Clinical Acupuncture and Moxibustion, (04),9-11. doi:CNKI:SUN:ZJLC.0.2014-04-005.