Acupuncture plus herbs benefit elderly patients with functional constipation. Researchers from the Third Affiliated Hospital of Zhejiang Chinese Medical University conducted a randomized controlled clinical trial and confirmed that the combined protocol of acupuncture plus herbal medicine produces superior outcomes to using Duphalac monotherapy (i.e. lactulose, a synthetic sugar used to treat chronic constipation) to control functional constipation in elderly patients. [1]
The complete spontaneous bowel movements (CSBMs) score demarcates significant improvements, measured at the twelve-week data point after completion of an eight-week regimen of acupuncture plus herbs therapy. In addition, the patient assessment constipation-quality life questionnaire (PAC-QOL), Bristol stool character scores, and assessment results of difficulty in defecation all improved significantly compared with the lactulose control group.
A total of 138 patients participated in the trial. Patients were randomly divided into an acupuncture group and a medication group, with respectively 65 and 73 patients in each group. For the treatment group, a specific acupuncture point prescription and herbal medicine formula were prescribed based on different diagnostic patterns. The primary acupoints selected were the following:
- ST25 (Tianshu)
- CV4 (Guanyuan)
- TB6 (Zhigou)
- ST37 (Shangjuxu)
Additional acupoints were selected based on an individual TCM diagnostic patterns. For qi deficiency, the following acupoints were added:
- SP15 (Daheng)
- CV8 (Shenque)
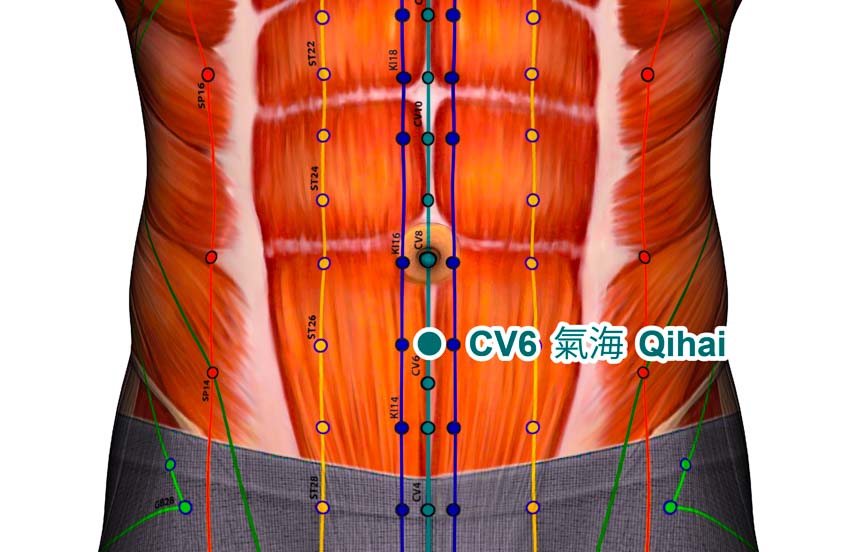
- CV6 (Qihai)
- ST36 (Zusanli)
- BL25 (Dachangshu)
For yin deficiency, the following acupoints were added:
- SP6 (Sanyinjiao)
- KI3 (Taixi)
- KI6 (Zhaohai)
- BL23 (Shenshu)
- BL25 (Dachangshu)
For yang deficiency, the following acupoints were added:
- CV8 (Shenque)
- ST36 (Zusanli)
- GV4 (Mingmen)
- BL23 (Shenshu)
- BL25 (Dachangshu)
For qi stagnation, the following acupoints were added:
- CV12 (Zhongwan)
- CV10 (Xiawan)
- SP14 (Fujie)
- BL57 (Chengshan)
- LI4 (Hegu)
- LV3 (Taichong)
For excessive heat, the following acupoints were added:
- CV12 (Zhongwan)
- CV10 (Xiawan)
- SP14 (Fujie)
- LI11 (Quchi)
- ST34 (Liangqiu)
- BL57 (Chengshan)
Patients were first instructed to rest in a supine position for acupuncture needles applied to the ventral aspect of the body. After disinfection of the acupoint sites, a 0.25 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. Manual acupuncture stimulation techniques were applied based on diagnostic patterns.
For patients with deficiency patterns, the tonifying (Bu) technique was used, and moxibustion was applied to CV8 (Shenque) for 20 minutes. For patients with excess patterns, the attenuating technique was used. Once a deqi sensation was obtained, the needles were retained and moxibustion was applied. A 30-minute needle retention time was observed.
Next, the dorsal acupoints were treated. After insertion of filiform needles into BL25 (Dachangshu), BL23 (Shenshu), and GV4 (Mingmen), the needles were manipulated for two minutes before withdrawal. No needle retention time was required.
For Yang deficiency patients, moxibustion was applied at Mingmen and Shenshu for 20 minutes. Acupuncture plus moxibustion therapy was conducted three times per week, for the duration of eight weeks. The treatment group patients also received modified Zhi Zhu Tang as a primary herbal formula, including the following ingredients:
- Zhi Shi 20 g
- Bai Zhu 60 g
Additional herbal formulas were prescribed based on diagnostic patterns. For qi deficiency patients, the modified herbal formula of Bu Zhong Yi Qi Tang was prescribed, which contained the following herbs:
- Huang Qi 30 g
- Chen Pi 5 g
- Sheng Ma 9 g
- Chai Hu 9 g
- Dang Gui 20 g
- Che Qian Zi 10 g
- Zhi Gan Cao 10 g
For yin deficiency, the herbal formula modified Liu Wei Di Huang Tang was prescribed:
- Sheng Di 12 g
- Shu Di 12 g
- Shan Zhu Yu 15 g
- Shan Yao 15 g
- Ze Xie 10 g
- Fu Ling 10 g
- Dan Pi 10 g
- Bai Shao 20 g
- Gua Lou Ren 15 g
For Yang deficiency, the herbal formula modified Ji Chuan Jian was prescribed:
- Rou Cong Rong 15 g
- Ze Xie 10 g
- Sheng Ma 5 g
- Zhi Ke 15 g
- Dang Shen 15 g
- Gan Jiang 10 g
- Zhi Gan Cao 10 g
For qi stagnation, the herbal formula modified Liu Mo Tang was prescribed:
- Bing Lang 10 g
- Chen Xiang 10 g
- Mu Xiang 10 g
- Wu Yao 10 g
- Hou Po 10 g
- Zhi Gan Cao 6 g
For excessive heat, the herbal formula modified Ma Zi Ren Tang was prescribed:
- Huo Ma Ren 15 g
- Bai Shao 15 g
- Tao Ren 12 g
- Hou Po 12 g
- Zhi Gan Cao 6 g
The above ingredients were brewed with water to obtain a 200 ml decoction, which was then split into 2 servings, taken separately in the morning and at night. Patients consumed the TCM herbal medicine for eight consecutive weeks, and a total of 56 servings were administered.
The results indicate that acupuncture with herbs is more effective than the prescribed non-absorbable synthetic sugar medication. Shi et al. demonstrate that acupuncture is safe and effective for the treatment of functional constipation. Based on a 12-week follow-up, researchers conclude that the TCM protocol demonstrates superior positive patient outcomes in both short and long-term results without any significant adverse effects. At HealthCMi, we would like to see another study to confirm the results with a third arm combining both approaches to patient care.
Reference:
[1] Shi YC, Wang C, Wang LY, et al. (2017). Complex Treatments of Acupuncture and Chinese Herbal Medicine Based on Syndrome Differentiation for Senile Functional Constipation: A Randomized Controlled Trial. Journal of Zhejiang Chinese Medical University, 41(06), 464-470.