Acupuncture and herbs are shown effective for the treatment of COVID-19 in modern research. In one investigation, acupuncture plus herbal medicine produced significant outcomes for severe COVID-19 patients. In another independent investigation, acupuncture and herbs alleviated symptoms for COVID-19 patients. The results were confirmed with CT scans. Let’s take a look at both investigations.
Acupuncture plus herbs produces significant patient outcomes for severe COVID-19 patients. A total of 17 patients from Wuhan Leishenshan Hospital participated in the study. [1] All patients in the study were diagnosed with severe-type COVID-19 from February 20 to March 29, 2020. There were 8 males and 9 females. The average age was 62 ±13 years. The average course of disease was 24.8 ±16.1 days. In addition to the Treatment Protocol for COVID-19 (Trial Version No. 7) published by the National Health Commission, patients with severe COVID-19 also met the following inclusion criteria:
- Shortness of breath, respiratory rate ≥30 breaths/min
- Resting oxygen saturation level ≤93%
- Arterial partial pressure (PaO2)/oxygen absorption concentration (FiO2) ≤300 mmHg (1 mm Hg = 0.133 kPa)
- Pulmonary imaging showing significant lesion progression >50% within 24–48 hours
All patients received acupuncture at the following acupoints:
- KD3 (Taixi)
- Daixie (代谢穴, Metabolic Point)
- Zhichuan (止喘穴, extra point)
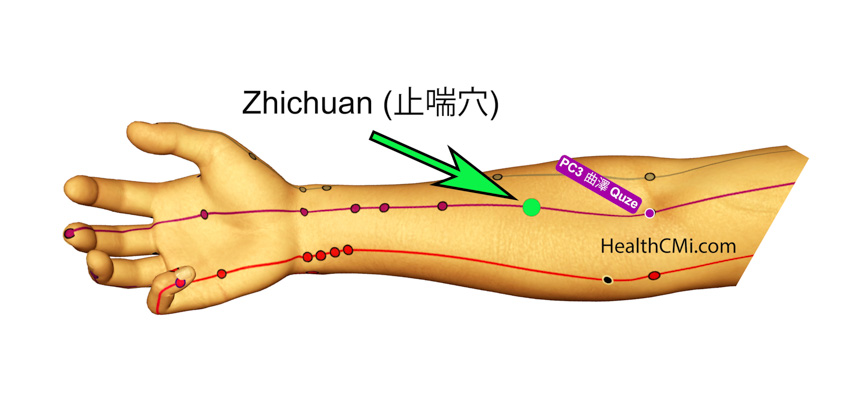
While KD3 is a standard acupoint, both Zhichuan and Daixie are less common. Zhichuan is located on the medial aspect of the forearm on a line connecting PC3 (Quze) and PC7 (Daling). Zhichuan is located at the upper third of this line, between the wrist crease and the transverse cubital crease. Indications for use of Zhichuan are myocardial disease, rapid heart rate, chest tightness, shortness of breath, and congestive heart failure.
Zhichuan is an extra point located along the pericardium channel, which explains its relevance to the heart. In addition, its use for COVID-19 patients is based on the stages of disease progression. Initially, external pathogenic diseases often affect the lungs and the taiyang channels. Eventually, diseases may progress to the jueyin level (liver, pericardium). The addition of Zhichuan to the acupoint prescription, according to HealthCMi educators, is intended to prevent the progression of the illness to critical stages and to prevent the invasion of fire-poison from the exterior to the interior.
Daixie is an extra point located 8 cun above KD3, posterior to the medial border of the tibia, in the depression between the medial border of the tibia and the gastrocnemius muscle. Its close proximity to LV6 (Zhongdu), indicates a potential for preventing progression of illness to the jueyin stage. Its location between SP7 (Lougu) and SP8 (Digi) indicates a potential for benefitting the spleen qi. Since both LV6 and SP8 are xi-cleft acupoints, Daixie may be well-suited for the treatment of acute diseases.
Additional acupoints were administered based on different symptoms. For fever, the following acupuncture points were added:
- LI4 (Quchi)
- LI11 (Hegu)
For turbid phlegm, the following acupuncture point was added:
- ST40 (Fenglong)
For chest tightness, the following acupuncture point was added:
- PC6 (Neiguan)
For general soreness, the following acupuncture point was added:
- TB5 (Waiguan)
Patients were treated in either the supine or seated position. Upon disinfection, a 0.25 mm x 40 mm disposable acupuncture needle was inserted, reaching a depth of 10–20 mm. After achieving a deqi sensation, needles were manipulated using different techniques, based on differential diagnostic patterns. For excess patterns, the tonifying (bu) technique was used. For deficiency patterns, the attenuating (xie) technique was used. For intermingling deficiency and excess, the mild tonifying and attenuating (ping bu ping xie) technique was used. The above acupuncture therapy was administered once per day until discharge.
Herbal formulas were also prescribed for different patterns. For excess patterns, either of the following formulas was given: Jie Biao Xuan Fei decoction, Jie Biao Qing Li decoction (i.e., Ma Xing Shi Gan decoction), Xue Bi Jing Injection (a Chinese patent drug), or a modified version of Da Chai Hu Tang. For deficiency patterns, Si Ni San was administered in addition to herbs that tonify the spleen and stomach and strengthen spleen qi.
Acupuncture plus herbal medicine achieved a total effective rate of 82.4% for the treatment of severe COVID-19. After treatment, the oxygen saturation levels of all patients significantly improved compared with readings before treatment. A total of 50–75% of the patients no longer had the following symptoms: fever, dry cough, fatigue, shortness of breath, chest tightness, cough, dry mouth, and loss of appetite. CT scans showed significant improvements in 41.2% of the patients after completion of this study. Seven out of 17 cases had complete resolution of lung abnormalities, shown on CT imaging.
Liu et al. had similar results in their independent investigation. [2] The researchers observed the effect of TCM treatment (including herbal medicine and acupuncture) for 17 patients with COVID-19. Before treatment, X-ray examinations showed that all patients presented with ground-glass opacities, 11 patients with partial consolidation, 10 with interstitial changes, and one patient with pleural effusion. After treatment, 15 cases showed obvious improvements on lung imaging. One month later, 12 patients were discharged, 3 patients were transferred, and 2 patients remained hospitalized (because of positive COVID-19 tests in fecal samples).
Formulas were prescribed for specific diagnostic considerations. For damp-toxin stagnation in the lungs, a modified version of Ma Xing Yi Gan decoction or Ping Wei powder was used. For cold-dampness obstruction in the lung, a modified version of Da Yuan Yin or Xiao Qing Long Tang was used. For epidemic-toxicity blocking the lung, a modified version of Ma Xing Shi Gan Tang or Huo Pu Xia Ling Tang was used.
The following acupoints were used for acupuncture treatment: LU9 (Taiyuan), SP4 (Gongsong), and ST36 (Zusanli). The researchers concluded that TCM treatment significantly improves symptom scores as well as chest imaging results for COVID-19 patients, but they also suggest that large scale randomized controlled studies are needed to confirm the existing findings.
References:
[1] Yin X, Cai SB, Chen LM, Zhang ZD, Guo LH, Zou X. (2021). Combination of acupuncture and herbs medicine for the treatment of 17 severe COVID-19 cases (in Chinese). Chinese Acupuncture and Moxibustion, 41(05):498-500.
[2] 26. Liu X, Qiao S B. (2020). Preliminary analysis of clinical characteristics and curative effect of 17 cases of novel coronavirus pneumonia treated by integrated traditional Chinese and Western medicine (in Chinese). Asia-Pac Tradition Med,16(06):1–5.


