Clinical trials demonstrate that acupuncture and herbs alleviate post-stroke hemiplegia. Researchers from the Third Affiliated Hospital of Henan University of Chinese Medicine investigated the effects of acupuncture and traditional herbal medicine on post-stroke hemiplegia. They concluded that the combination of both TCM (traditional Chinese medicine) modalities is a more effective treatment protocol than using only acupuncture. Acupuncture combined with herbs yielded an 88.0% total effective rate and using only acupuncture had a 74.83% total effective rate. [1]
In TCM, post-stroke hemiplegia is often due to the imbalance of yin and yang, and the improper qi and blood flow into the brain. TCM states the treatment principle is to regulate qi and blood by dredging the meridians. Professor Shi Xuemin from China Academy of Engineering established a protocol called the Xing Nao Kai Qiao (brain-wakening and orifice-opening) acupuncture method. Modern research has shown that this method is effective for post-stroke patients by increasing nourishing blood flow in the brain, relieving nerve cell damage, and improving blood viscosity. [2] Another TCM therapeutic approach extensively used for post-stroke treatment is the herbal formula Bu Yang Huan Wu Tang. In this study, both methods were tested for their efficacy in treating post-stroke hemiplegia.
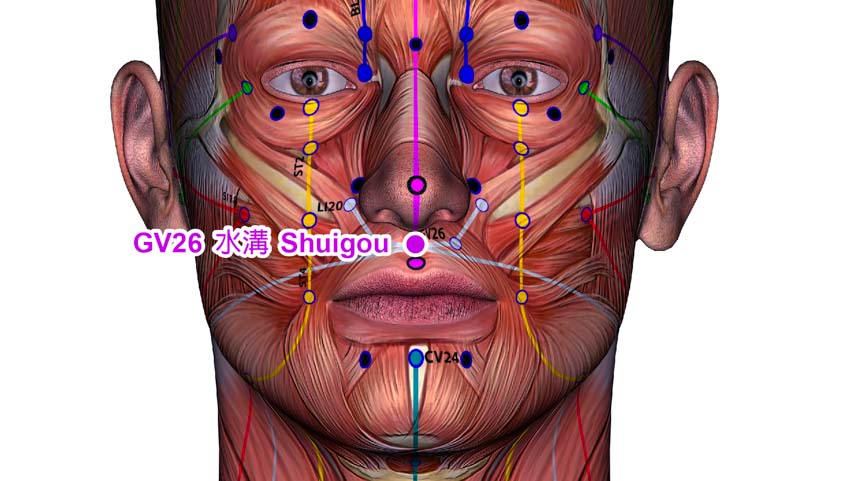
A total of 100 patients were randomly divided into two groups: treatment group, control group. The control group was given only acupuncture and the treatment group was given both acupuncture and Bu Yang Huan Wu Tang for treatment. For the Xing Nao Kai Qiao acupuncture therapy, the selected primary acupoints were the following:
- GV26 (Renzhong/Shuigou)
- PC6 (Neiguan)
- SP6 (Sanyinjiao)
- LU5 (Chize)
- HT1 (Jiquan)
- BL40 (Weizhong)
After standard disinfection, a disposable needle was swiftly inserted into each acupoint with a high entry speed. For Renzhong, the needle was inserted obliquely in the direction of the nasal septum, reaching a depth of 0.3 – 0.5 cun. A sparrow-pecking technique was used to achieve an eye-moistening effect for patients and no needle retention was needed.
For Neiguan, the needle was inserted perpendicularly to a depth of 0.5 – 1.0 cun. The xie (attenuating) technique was used. For Sanyinjiao, the needle was inserted perpendicularly to a depth of 0.8 – 1.5 cun and the bu (tonifying) technique was used. For Jiquan, the needle was inserted perpendicularly to a depth of 0.5 – 0.8 cun and the xie (attenuating) technique was used. For Chize and Weizhong, the needle was inserted perpendicularly to a depth of 0.5 – 1.0 cun and the xie (attenuating) technique was used. All manipulation techniques were applied for one minute or until three occurrences of muscle twitching were observed at the acupuncture site.
One acupuncture session was conducted once per day. A full treatment cycle consisted of six days, followed by a one-day break. The entire treatment course was comprised of four treatment cycles. A total of three treatment courses were conducted. The mandatory ingredients used in the modified Bu Yang Huan Wu Tang were as follows:
- Huang Qi 60g
- Dang Gui Wei 6g
- Chi Shao 5g
- Di Long 3g
- Chuan Xiong 3g
- Tao Ren 3g
- Hong Hua 3g
Additional herbs were added based on individual symptoms. For patients with qi deficiency, Dang Shen was added. For patients with blood stasis, San Ling and E Zhu were added. For patients with deviation of the mouth and eyes, Jiang Can and Quan Xie were added. For speech impairment, Chang Pu and Yuan Zhi were added. For phlegm-heat, Zhi Shi and Gua Lou were added. For excessive phlegm, Ban Xia was added. For painful limbs, Ji Xue Teng was added.
The prescribed ingredients were brewed with water to make an herbal decoction. One decoction was separated into two doses, one taken in the morning and one at night. The Chinese herbal medicine treatment lasted for a grand total of 12 weeks. Treatment efficacy was categorized into 4 tiers:
- Recovery: The National Institute of Health Stroke Scale (NIHSS) score decreased by 91% to 100%.
- Significantly effective: The NIHSS score decreased by 46% to 90%.
- Effective: The NIHSS score decreased by 18% to 45%.
- Ineffective: The NIHSS score decrease by less than 18%.
After treatment, the Fugl-Meyer Assessment (FMA) scores in upper and lower limbs,Brunnatrom grading,functional ambulation category scale (FAC) scores,Barthel index and Short Form 36 Health survey Questionnaire (SF-36) scores in both groups were significantly higher than those before treatment, and the improvement in the treatment group was higher than that in the control group.
Furthermore, the levels of C-reactive protein (CRP), nitric oxide (NO) and homocysteine (Hcy) measured 7 and 14 days after treatment in both groups were significantly lower than those before treatment, and the improvement in the treatment group was higher than that in the control group. The results indicate that acupuncture with herbs is more effective for the treatment of post-stroke hemiplegia than using only acupuncture.
References:
[1] Zuo G, Ren CY, Wu YM, Li SS. (2019). Clinical Study on Xingnao Kaiqiao Acupuncture Combined with Buyang Huanwu Tang for Poststroke Hemiplegia. Journal of New Chinese Medicine, 51(09):234-237.
[2] Wen K, Zhu HC, Yuan H, et al. (2016). Effect of Different Application Timing of Xing Nao Kai Qiao Acupuncture on Cognitive Dysfunction in Patients with Acute Cerebral Infarction. Journal of Integrated Traditional Chinese and Western Medicine, 25(26): 2875- 2878.


