Acupuncture combined with herbal medicine is effective for the treatment of post-stroke aphasia. In one investigation, acupuncture plus herbal medicine produced superior treatment outcomes when compared with intravenous injections of edaravone. In another investigation, acupuncture plus speech therapy was found superior to using only speech therapy. Aphasia is a condition caused by brain damage that affects the ability to communicate through speech or written language. This affects both comprehension and expression.
Researchers (Wang et al.) from Heyang County Chinese Medicine Hospital confirmed that a protocol of acupuncture plus herbal medicine is more successful than a protocol of edaravone injections when treating post-stroke aphasia. [1] Wang et al. conclude that acupuncture plus herbs achieved a 92.94% total treatment effective rate. Edaravone injections achieved a 75.29% total treatment effective rate. Acupuncture plus herbs outperformed edaravone by 17.65%. Given the data, the professors at HealthCMi would like to see an additional arm of a study using a combination of edaravone plus acupuncture to determine if this improves clinical outcomes to an even greater degree than either monotherapy.
A total of 170 patients were treated and evaluated in the study. They were randomly divided into two groups: an acupuncture plus herbs treatment group and an edaravone control group, with 85 patients in each group. The treatment group was treated with acupuncture (tongue acupuncture and body acupuncture) and an herbal formula, while the control group was treated with edaravone intravenous injections. Edaravone is a drug used to alleviate oxidative stress and protect neurons.
The treatment group patients received tongue acupuncture, body acupuncture, and herbal medicine. For tongue acupuncture, the points Juquan (Ex-HN10), Jinjin (EX-HN12), and Yuye (EX-HN13) were used. Juquan (Ex-HN10) is located at the midpoint of the tongue midline, when the tongue is outstretched. Jinjin and Yuye are paired points on the veins lateral to the frenulum of the tongue. Jinjin is on the patient’s left side and Yuye on the right. To locate these points on the underside of the tongue, use a tongue depressor or gauze to roll back the tongue.
Needles were inserted into the tongue acupuncture points and immediately withdrawn. No retention of needles was administered for the tongue points. For body acupuncture, the following acupoints were selected for treatment:
- Sishencong (HN-1)
- GV20 (Baihui)
- LI4 (Hegu)
- LI11 (Quchi)
- SP10 (Xuehai)
- ST36 (Zusanli)
- HT5 (Tongli)
- KD3 (Taixi)
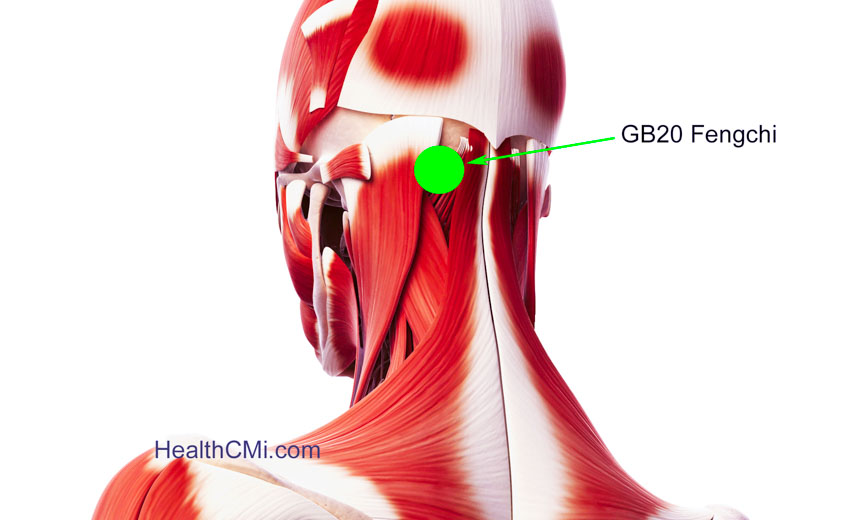
- GB20 (Fengchi)
After standard insertion, needles were inserted into each point with a high needle entry speed. For Sishencong and Baihui, the piercing (touci) acupuncture technique was used. For the rest of the points (Hegu, Quchi, Xuehai, Zusanli, Tongli, Taixi, and Fengchi), the perpendicular needle insertion technique was used. For one month, one 30-minute electroacupuncture session was conducted daily. The herbal formula given to the treatment group was comprised of the following herbs:
- Shu Di 30 g
- Niu Xi 30 g
- Sheng Huang Qi 25 g
- Shan Zhu Yu 15 g
- Shi Chang Pu 15 g
- Yuan Zhi 15 g
- Yu Jin 10 g
- Ze Xie 10 g
- Fu Ling 10 g
- Bai Li Ji 10 g
- Dan Nan Xing 10 g
Additional herbs were prescribed according to individual symptoms. For extremity numbness, Di Long and Jiang Can were added. For gurgling phlegm and excessive saliva, Chen Pi and Ban Xia were added. For reluctance to speak due to qi deficiency, Tai Zi Shen and Bai Zhu were added. A decoction was made from fresh herbs each day, divided into two parts, and administered in two servings (one in the morning and one at night).
In an independent research trial, Kong et al. from Henan Kaifeng Central Hospital investigated the treatment efficacy of acupuncture combined with speech therapy (ST) for post-stroke aphasia patients. The researchers determined that acupuncture with ST yielded better treatment results than using ST as a standalone therapy. Acupuncture plus ST achieved a 91.75% total treatment effective rate, while using only ST achieved a 68.57% total treatment effective rate. [2]
A total of 70 patients were treated and evaluated in the study. They were randomly divided into a treatment group and a control group, with 30 patients in each group. The treatment group underwent acupuncture with ST while the control group received only ST. The acupuncture treatment was comprised of three parts: scalp acupuncture, body acupuncture, and bleeding technique acupuncture.
For scalp acupuncture, the areas Speech I, Speech II, and Speech III were selected. Upon disinfection, a 0.30 mm x 40 mm disposable filiform needles were inserted into each acupuncture site with a high needle entry speed. After obtaining deqi, needles were rotated for one minute with a frequency of 120 r/min. Next, the needles were connected to an electroacupuncture device with a 10 Hz continuous wave. The needles were retained for 30 minutes. One electroacupuncture session was conducted daily, for a total of 45 days.
For body acupuncture, the primary acupoints selected were the following:
- CV23 (Lianquan)
- GV26 (Renzhong)
- GV24 (Shenting)
- GV20 (Baihui)
- GV15 (Yamen)
- KD1 (Yongquan)
Upon arrival of a deqi sensation, twisting, lifting, and thrusting manual acupuncture techniques were applied. A needle retention time of 30 minutes was observed, during which the needles were manipulated for one minute every 10 minutes (three times). The body acupuncture treatments were administered for 45 days.
Bleeding technique therapy is an ancient acupuncture technique. It is mainly used for invigorating the smooth flow of qi and blood. In this study, this acupuncture technique was performed at Jinjin (EX-HN12) and Yuye (EX-HN13). A three-edged needle was used to pierce varicose veins at the acupoints to release small amounts of blood. The treatment was administered every two days, with 15 days as one course of treatment, for a total of three treatment courses.
The researchers concluded that acupuncture combined with ST is more effective than using ST alone for the treatment of post-stroke aphasia, especially in improving patients’ ability to talk, paraphrase, and comprehend language. Both studies reviewed in this article demonstrate that acupuncture is an effective therapy for relief from post-stroke aphasia. Given the data, acupuncture and other TCM modalities are recommended as viable treatment options for treating post-stroke aphasia.
References:
[1] Wang HY, Wei J. (2018). Effect of traditional Chinese medicine oral administration combined with acupuncture on aphasia after ischemic stroke. Clinical Research and Practice, 24(3): 90-91.
[2] Kong HT. (2018). Observation on the curative effect of acupuncture combined with speech therapy in the treatment of post-stroke aphasia. Journal of Practical Chinese Internal Medicine, 34(3): 359.


