Acupuncture plus electroacupuncture has been proven effective for the treatment of peripheral facial paralysis (PFP). This condition is also termed Bell’s palsy. In a recent study, researchers from Guangzhou University of Traditional Chinese Medicine (Clinical Medical College of Acupuncture, Moxibustion, and Rehabilitation) conducted a clinical experiment. They compared warm needle acupuncture monotherapy with warm needle acupuncture plus electroacupuncture. The combined treatment protocol demonstrated superior patient outcomes. [1]
The results show that the total rate of clinical efficacy was 94.74% in the integral group, which was significantly higher than that of the control group (warm needle monotherapy) at 87.18%. The efficacy rate in the study was based on the House-Brackmann Facial Paralysis Scale (HBGS). Patients at HBGS level 1 with normal facial symmetry were classified as recovered. Those with HBGS level improved by at least two levels, facial symmetry when staying still, near facial symmetry while moving facial muscles, and fewer than two facial muscle disorders were classified as significantly effective. Those with HBGS level improved by one level, facial symmetry when staying still, near facial symmetry while moving facial muscles, and more than two minor facial muscle disorders were classified effective. Those presenting no improvement were classified ineffective.
Sunnybrook Facial Grading System ( SBGS) scores in both groups increased, with the higher rise shown in the integral group from 36.68 ±3.27 to 78.61 ±4.03. A more considerable decline in Facial Disability Index about Social Function (FDIS) was observed in the integral group, dropping from 15.34 ±4.47 to 6.61 ±1.31.
Researchers demonstrate that the integral approach markedly relieved symptoms of PFP and positively benefitted patients’ mental conditions associated with the disorder. Electro-needling showed no evidence of adverse effects and did not aggravate facial neuroinflammation. As a result, the research team deemed the integrated protocol a safe and effective treatment method for the treatment of peripheral facial paralysis.
Eighty patients were admitted into the study. They were randomly divided into two groups, with 40 cases in each group. One received only warm needle acupuncture (moxa). The other group also had electroacupuncture. The statistical baselines were the same prior to the study in terms of gender, age, course of condition, House-Brackmann Facial Parasis Scale (HBGS), Sunnybrook Facial Grading System ( SBGS), and Facial Disability Index about Social Function (FDIS). These parameters considered measures of anxiety, loneliness, anger, and poor sleep quality.
All of the 80 patients received basic pharmaceutical treatment. Three prednisone tablets (5 mg/tablets) were administered twice daily. Vitamin B1 (10 mg/tablet) were given three times daily for one month. For the electroacupuncture group, needles (0.25 × 25 mm, 0.25 × 40 mm) were applied to the following acupoints:
- GB14 (Yangbai)
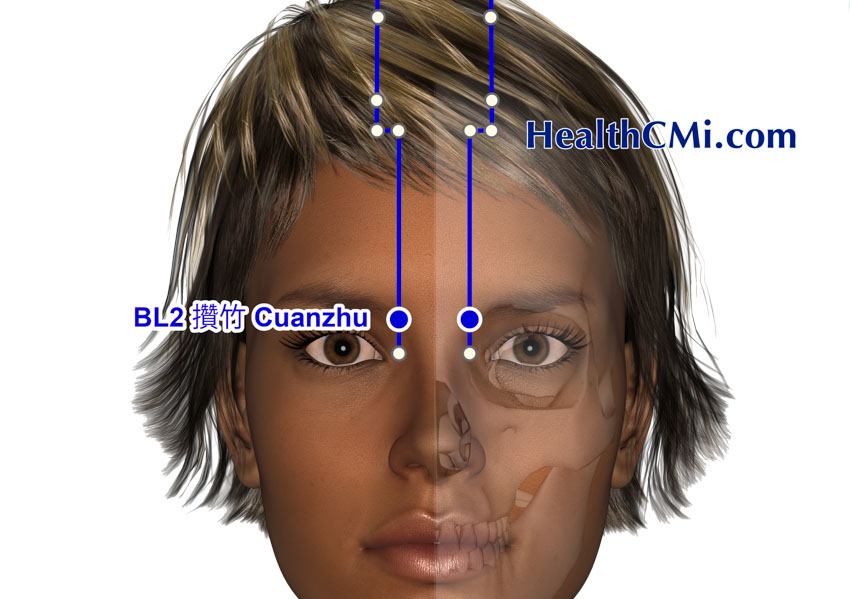
- BL2 (Cuanzhu)
- EX-HN5 (Taiyang)
- ST2 (Sibai)
- ST4 (Dicang)
- TB17 (Yifeng)
- LI4 (Hegu)
- ST7 (Xiaguan)
For all patients, upon achieving deqi, the mild reinforcing-attenuating manipulation technique was used. Warm needle acupuncture at Taiyang, Xiaguan, and Yifeng was applied. For each treatment session, two of the aforementioned points were used. Moxa pieces, two centimeters in length, were connected to the needle end. Duration and frequency of treatment were the same as in the electroacupuncture group.
In the electroacupuncture group, Yangbai, Sibai, Dicang, and Jiache were connected to an electroacupuncture device. Frequency was set at 2 Hz. A disperse-dense wave was used. Intensity was set low. The treatment lasted for 30 minutes per session (one per day), with five sessions and a two-day interval completing one course. Patients underwent three courses in total. The results demonstrate that an integrated protocol of warm needle acupuncture plus electroacupuncture increases positive patient outcomes.
Reference:
[1] Feng Jingyi, Zhang Zhiwen, Lao Jinxiong, Clinical Observation on Treating Peripheral Facial Paralysis with warm needle acupuncture, Act. Chinese Medicine and Pharmacology, Vol. 50, No. 9, Sept. 2022.