Acupuncture alleviates menstrual pain. Pinglu Hospital researchers conducted a controlled clinical trial comparing the efficacy of warm needle acupuncture and Chinese moxibustion versus ibuprofen for the relief of menstrual related discomfort. The acupuncture group outperformed the drug group with a total efficacy rate of 95.24% for the treatment of dysmenorrhea. [1]
Observational parameters used in the study were: a four-level pain scale (higher scores indicating more severe pain), a rating system for accompanying symptoms (including nausea, vomiting, loss of appetite, loss of sleep, back pain, cold limbs, cold sweats, fainting, pale complexion, etc., with higher scores signifying increased severity). In addition, uterine microcirculation was monitored by color ultrasound at T1 (prior to the treatment), and T2 (three months after the treatment). This quantified uterine arterial systolic blood flow velocity (Vs), uterine artery diastolic blood flow velocity (Vd), and average velocity (Vm).
In terms of symptom scoring, prior to the research, the figures for the two groups were approximately the same. Following completion of the treatment, a greater decrease in severity was observed in the warm needle acupuncture group, dropping from 11.21 ±2.31 to 4.85 ±1.62. All three parameters for uterine microcirculation improved more markedly in the acupuncture group. In the 42 cases in the ibuprofen group, 9 were significantly effective, 20 were effective, and 12 were ineffective. Total efficacy rate was 69.05%. In warm needle acupuncture group, 18 were significantly effective, 22 were effective, and 2 and were ineffective. Total efficacy rate was 95.24%.
The 84 cases were admitted into the hospital. The statistical baseline was the same at the outset. All patients had regular menstrual cycles and no organic obstruction in the reproduction organs. Visual Analog Scale (VAS) scores all exceeded four points. Those with severe cardiovascular, cerebrovascular pathology, and severe hepatic and renal dysfunction were excluded from the study.
For the drug group, patients were prescribed ibuprofen (0.3g) to be taken once or twice daily after the menstrual cycle started, depending on the severity of menstrual pain. For the acupuncture group, patients took a supine position and received frequent acupuncture treatments. The main acupoints used included the following:
- SP6 (Sanyinjiao)
- CV4 (Guanyuan)
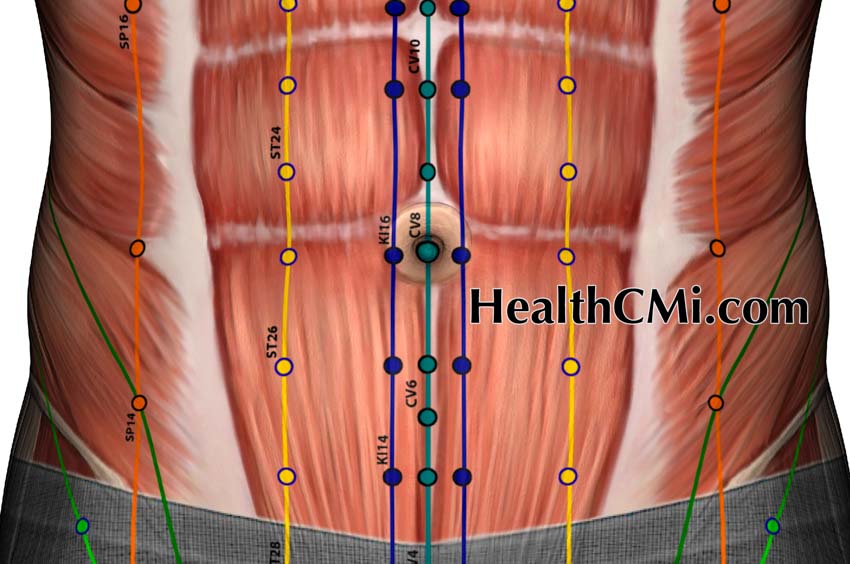
Supplementary points were selected based on patients’ individual conditions. For the blood stagnation and qi stasis type, SP10 (Xuehai) and BL32 (Ciliao) were added. For cold-dampness stagnation type, SP9 (Yinlingquan) and SP8 (Diji) were added. For qi and blood deficiency type, CV6 (Qihai) and ST36 (Zusanli) were added. For liver and kidney deficiency type, BL18 (Ganshu) and BL23 (Shenshu) were added.
Acupuncture needles were swiftly inserted to a depth of 15-25 mm. A deqi sensation was achieved through twisting and twirling the needles. Next, a mild reinforcing and attenuating technique was applied. Three moxa pieces, 2.5 centimeters in length, were connected to needle ends. Needle retention time was 30 minutes per acupuncture session. Simultaneously, moxa was applied to CV8 (Shenque). Both groups received treatment for a total of three menstrual cycles.
Patients receiving acupuncture had significantly superior outcomes for pain relief and improvements in uterine microcirculation. The researchers note that use of acupuncture avoids dependence on long-term medication use that may lead to harmful adverse effects, including gastrointestinal disorders. At HealthCMi, we would like to see a follow-up investigation with a third arm to the study wherein ibuprofen and warm needle acupuncture are combined in an integrated protocol to test for possible additive effects.
Reference:
[1] Shi Jianghong, Moxibustion on Shenque Combined with Warming Needle Moxibustion in the Treatment of 42 cases of Primary Dysmenorrhea, Guang Ming Traditional Chinese Medicine, March 2022, Vol 37, Issue 5.


