The Menstrual Cycle
Sample of Course Materials
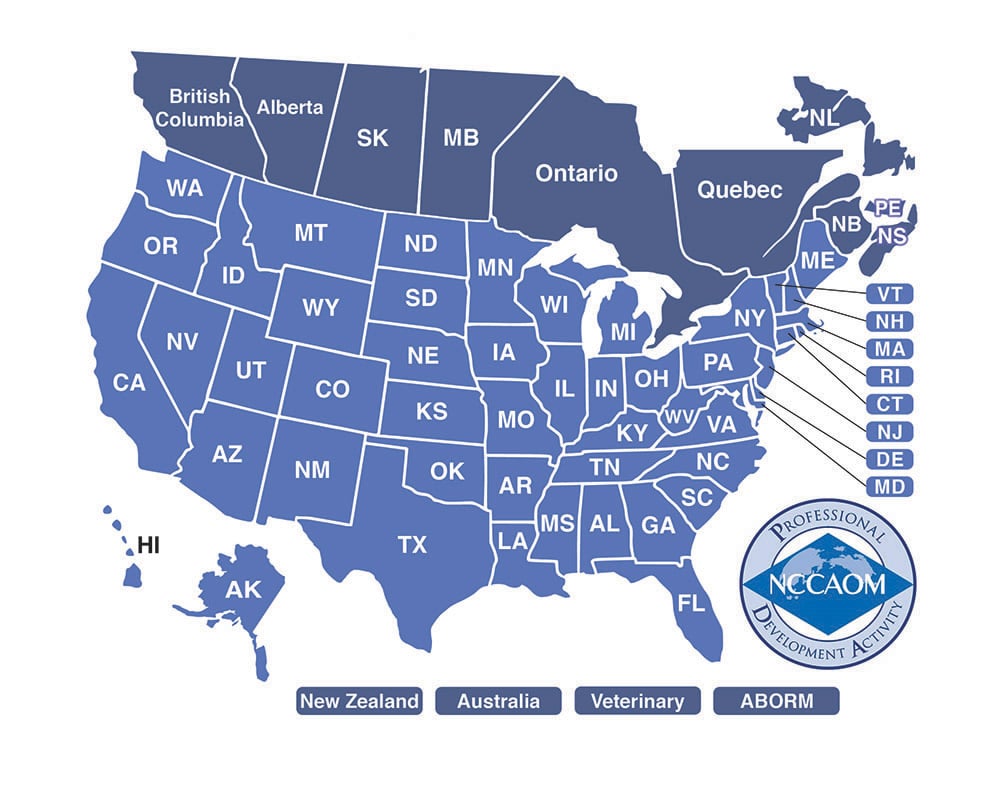
Credits: 8 Acupuncturist CEUs-PDAs-CAEs. Also: 8 California nurse contact hours. Download the course materials, complete the online quiz and receive immediate acupuncture license credit. Take a look inside the course materials in the samples below:
Sample #1 from the biomedicine section of the course material:
Prostaglandins—Prostaglandins are not hormones. They are a group of neurotransmitters with a huge effect on the female reproductive tissue such as oviductal and myometrial (uterine muscle) tissue. Prostaglandin actions are wide range including vasoconstriction, cytoprotection, and platelet aggregation to name a few. Excess levels of prostaglandins cause the smooth muscles of the endometrium to contract hence causing the menstrual pain we see in primary dysmenorrhea.
The following illustration shows the normal changes in endometrium and hormone levels throughout the menstrual cycle:

Sample #2 from the biomedicine section of the course material:
|
Phases of the Menstrual Cycle |
|
Menses Phase: Cycle day 1 – 3 or 4; can last up to 7 days |
|
Follicular Phase: Technically also includes days 1 – 4 and goes to cycle day 12 |
|
Ovulation Phase: Lasts hours occurs anywhere from cycle day 13 – 14 |
|
Luteal Phase: Post ovulation from cycle day 15 – 28 |
The average menstrual cycle is described as:
- 28 days long
- Luteal hormone surge circa day 12 – 13
- Ovulation at approximately day 14
- Menstruation two weeks following ovulation
- Complete shedding of the uterine lining
- Menstrual bleeding (periods) lasting 3 – 7 days
- No spotting before or between periods
- Free of blood clots
While it is true that every woman’s body is different—so the menstrual cycle may vary somewhat from individual to individual—some characteristics are considered normal (or baseline). The above characteristics are commonly considered average. Please note in some cases, a woman may have a 26 or 30 day cycle throughout her entire menstrual history, and this cycle length would be considered normal for her. As practitioners, we need to be flexible to some degree and base each situation on a case-by-case basis. Usually, however, too short cycle lengths may not provide sufficient time for eggs to mature or the short length may contribute to insufficient luteal phases (luteal phase defect, a common cause of infertility). On the other hand, in cases where the cycle lengths are too long, the patient may experience delayed menstruation, severe PMS, and infertility, as well. So, as you can see, having too long or too short cycles are both pathological. Moreover, cycle lengths less than 24 days or more than 32 days may indicate other gynecological problems, such as polycystic ovarian syndrome, metrorrhagia, or amenorrhea. As a rule of thumb, any menstrual cycle more than two or three days outside the average should be regulated.
A major process in the menstrual cycle occurs in the ovaries. This process is the recruitment and selection of an oocyte (egg/ovum) within the ovarian follicle. Even before the cyclic selection process (anthral follicular phase), oogenesis begins up to 240 – 290 days before ovulation and is in itself a very complex process. Recall that as a result of meiotic division, the primary oocyte is suspended in an inactive state after birth. Meiosis is not completed until much later during the monthly recruitment process. Also, recall that at birth both ovaries combined contain about 2 million oocytes, by puberty that number has declined to 200,000 to 300,000 and throughout a women’s lifetime only about 400 to 500 follicles will reach maturity and actually produce a secondary oocyte (ovum). Ovarian follicles are aggregates (conglomeration of cells) containing a single immature ovum, granulosa, and thecal cells. The development and release of the ovum occurs in response to circulating gonadotropins and varying levels of follicular stimulating and luteinizing hormones.
Follicular phase—The first stage of the menstrual cycle begins on Day 1 of menses and is called the follicular phase. The follicular phase results in a mature ovum (egg), which can later be fertilized or eliminated from the body if fertilization does not occur. The follicular phase involves recruitment of primordial follicles through a pre-anthral stage, selection of a dominant follicle through the anthral follicular stage, and continued meiotic division (remember meiosis produces gametes: sex cells) development of the egg through the pre-ovulatory follicular stage.
The following table shows the major changes occurring during follicular development:
|
Stages of Follicular Development |
|
Follicular Phase (includes ovarian cycle):
|
Ovulatory phase (mid-cycle)—Ovulation occurs when an ovary releases an ovum into the fallopian tubes in response to a surge of luteinizing hormone. Ovulation may occur on cycle day 13 but commonly occurs around cycle day 14 – 14.5. It is marked by a change in the cervical mucus (having an egg-white consistency) and in some women a slight lower abdominal pain in the region of the ovulating ovary. The left and right ovaries can alternate ovulation from month to month and in some women primarily one side (left or right) will ovulate more the than the other side. There is no rule of thumb regarding to which ovary will predominate. The pain felt around ovulation is called Mittelschmerz (from German literally meaning “middle pain”). About 20% of women will experience this pain, either with every cycle or intermittently.
Luteal phase—The luteal phase follows ovulation and is the time period in which fertilization and increased growth of the endometrium occurs. The luteal phase typically lasts from 11 to 17 days; however, some clinicians find that a luteal phase of at least 12 days is more conducive to fertility. Less than 10 days is considered a luteal phase defect (LPD). During the luteal phase, the corpus luteum (white body), which separates from released ovum, begins synthesizing progesterone to promote pregnancy. The corpus luteum will remain for about 2 weeks if pregnancy does not occur, and if fertilization does occur, the corpus luteum will continue to make progesterone for to up 8 weeks until placental production takes over the job of making progesterone. Fertilization commonly occurs within the fallopian tubes. If it does not occur, then the endometrium is shed marking the end of the luteal phase.
Menstruation—Menses (or menstruation, also called a menstrual period) refers to the phase during which the endometrium is shed and cyclic bleeding occurs. Menses on average lasts 3 to 4 days and commonly begins light and goes to a heavier flow, eventually tapering off the last day or so. In some women, menses may last up to 7 days. A menstrual period lasting more than 7 days is considered pathological. The average menstrual flow is 30 – 50 mL of blood. Some texts indicate that a flow greater than 80 mL should be referred for medical evaluation. US Food and Drug Administration recommends changing tampons or pads at least every 4 to 6 hours using the lowest absorbency product for an individual’s flow. In clinical practice, a rule of thumb is the patient should not have to change the feminine hygiene product every two or three hours.
The US Department of Health and Human Services recommends a woman sees seeks medical attention if:
- Menstruation does not begin by the age of 15.
- Menstruation does not begin within 3 years after breast development, or if breasts haven't started to develop by age 13.
- Menstruation suddenly stops for more than 90 days.
- Menstrual periods become very irregular after having had regular, monthly cycles.
- Menstrual periods occur outside a 21 to 35 day frequency.
- Bleeding persists for more than 7 days.
- Bleeding is more heavy than usual or requires changing a pad or tampon every 1 to 2 hours.
- Bleeding occurs between menstrual periods.
- Severe pain accompanies the menstrual period.
- A woman gets a fever and feels sick after using tampons
Sample from the Chinese Medicine section of the course material:
TCM Treatment of Menstrual Disorders
This section covers TCM treatment for three common menstrual disorders: amenorrhea, oligomenorrhea and dysmenorrhea. Within the topic of dysmenorrhea, heavy bleeding is also addressed (as related to qi deficiency).
Several keys to treating menstrual disorders is to conduct a thorough medical history/patient intake, to take the time to differentiate, and to regularly to update the patient’s health history and diagnosis. Another important point regarding treatment is that it takes at least three cycles to regulate blood flow through the Ren and Chong. From the onset, the acupuncturist should express to the patient treatments will need to be administered two to three times weekly for at least three month for optimal effect. This is the frequency the author of this course recommends.
Amenorrhea and Oligomenorrhea
A TCM view of amenorrhea is the patient is experiencing a disruption of her bio-clock rhythm. Normal menstruation is viewed as monthly accumulation and release of yue xin (energy). When a woman fails to have a period (excluding pregnancy, menopause, and breastfeeding), typically from the TCM it is due to a congenital deficiency if the amenorrhea is primary or a secondary set of pathologies. In other words,
- Primary amenorrhea—Due to a congenital deficiency of Essence. This happens when a girl fails to menstruate, usually by age 14 according to the Nei Jing.
- Secondary amenorrhea—Due to a variety of causes:
- Trauma, surgery, etc. leading to blood stasis
- Emotional issues causing Liver Qi stagnationà Blood stasis
- Poor nutrition/irregular diet leading to dampness and phlegm retention blocking the Chong
- Poor nutrition leading to blood deficiency
- Overwork leading to Qi and Blood deficiency
- Cold accumulation in the uterus or attacking Shaoyin level
- Chronic, gradual onset of no menses, patient may have abdominal cramps.
- Sudden onset of no period, history of regular periods, no abdominal cramps
The Liver, Chong, and Uterus are important organs involved with menstruation via connection with endocrine function, blood storage, and qi and blood flow. Therefore, if there are any imbalances in those organs, amenorrhea may result. Kidney deficiency may also contribute to amenorrhea via the Kidneys influence on hormone levels. Both the Kidney and Liver should be addressed when regulating hormonal levels. For endocrine issues excesses indicate a more Liver imbalance, while deficient symptoms commonly point more to Kidney deficiency.
Pregnancy Note
Before treating amenorrhea, always rule out any possibility of pregnancy. Here’s a quick guide to help discern if your patient might be pregnant:
Differential Diagnosis of Amenorrhea vs. Pregnancy
|
Amenorrhea |
Pregnancy |
|
Symptoms Chronic, gradual onset of no menses, patient may have abdominal cramps. |
Sudden onset of no period, history of regular periods, no abdominal cramps |
|
Pulse Could be wiry; choppy; hesitant; deep, weak and thin |
Slippery |
|
Physical Examination No obvious gynecological changes |
Breast distension, darker nipples |
Acupuncture for Amenorrhea and Oligomenorrhea—When treating amenorrhea, the practitioner may use various points. The plan should involve regulating the Ren and Chong in all cases.
Sample from the Chinese Medicine section of the course material:
Pattern Differentiation
Qi and Blood Xu-- History of chronic illness, no menarche or irregular periods, fatigue, shortness of breath, poor appetite, poor memory, blurred vision, pale face, palpitations
T – Pale, thin white coat
P –Thready or thin, weak
Qi Stagnation and Blood Stasis—Irregular cycles, lots of clots, dark colored blood, pain, emotional issues, anxiety, depression, stress, anger, breast distension, mood swings, cramping, hypochondriac pain
T – Normal or purple with spots
P – Wiry or choppy
Damp and Phlegm Retention—May be overweight (Note: some patients may be thin or average weight and still have this pattern), abdominal distension, gas and bloating, mucus, vaginal discharge, phlegm, chest distension (from phlegm), sweaty palms
T – Pale, thick greasy white coat, moist
P – Slippery
Cold Accumulation in Uterus—Cold hands and/or feet, cold feeling, relieved by warmth, delayed menses with cramps, dark or black blood, large clots, severe pain, may have chill/fever, pale complexion
T – Pale, thin white coat or normal
P – Deep, slow, weak or tight
KID and LIV Yin Xu/ Essence Xu (deficiency) —Age 18 or older with no menarche, delayed overall growth, hair loss, hearing problems, weak knees/lower back pain, patient may have Yin Xu signs.
T – Pale, thin white coat
P – Deep, thin, weak in rear
Sample from the Chinese Medicine section of the course material:
Acupuncture
Basic points
- Ren 5 – Induces menses (NOTE: Avoid deep needling and during the period)
- Ren 6 – Regulates Qi; tonifies Qi, Yang and Yuan Qi
- Zigong – Extra point for uterus
- ST 28 – Promotes Qi flow
- SP 6 – Major gynecological point, Yin, blood, dampness
- Kid 8 – Endocrine point
- P 6 – Calms the mind, regulates blood
For Deficiency (Xu) patterns—Tonify the Ren and Chong using LU 7 and/or SP 4.
For Excess patterns— Drain excess with LU 7 + KD 6 and/or SP 4 + P6 using a cross insertion pattern to regulate the Ren and Chong.
KID and LIV Yin Xu/ Essence Xu (deficiency) —Tonify KID and LIV use basic points plus:
- KID 3 – Tonifies the Kidneys, nourishes the Essence, regulates the uterus, treats low back pain
- KD 6 – Nourishes Yin, cools blood, calms the mind, regulates the uterus
- BL 23 – Tonifies the Kidneys, nourishes the Essence
- BL 52 – Tonifies the Kidneys, psycho-emotional support
- GB 39 – Nourishes the Essence
- BL 18 – Benefits the Liver and Gallbladder
- LV 8 – Nourishes Liver Blood
- Ren 4 – Nourishes Yin and blood, Strengthens Yang, tonifies Kidney and Yuan Qi, regulates the uterus and menses
Qi and Blood Xu —Tonify Qi and nourish blood basic points plus:
- ST 36 – Tonifies Qi and blood
- LV 8 – Nourishes Liver Blood
- BL 17 –Tonifies blood and Qi, moves stagnant blood
- BL 18 – Benefits the Liver and Gallbladder
- BL 20 – Tonifies Spleen Qi and Spleen Yang
- Ren 4 – Nourishes Yin and blood, Strengthens Yang, tonifies Kidney and Yuan Qi, regulates the uterus and menses
Qi Stagnation and Blood Stasis—Soothe and regulate LIV, Move Qi and blood, Regulate Chong and Ren by draining excess plus may also use:
- LI 4 – Promotes Qi circulation, unblocks the channels
- LV 3 – Promotes Qi circulation, especially Liver Qi
- GB 34 – Unblocks channels, promotes Qi circulation
- SP 10 – Cools blood, moves blood
- BL 17 – Tonifies blood and Qi, moves stagnant blood
- BL 18 – Benefits the Liver and Gallbladder
- BL 19 – Relaxes the diaphragm, reduces stuffiness in the chest
- LV 13 – Promotes Qi circulation, especially Liver Qi, benefits the Stomach and Spleen
- LV 14 – Promotes Qi circulation, benefits the Stomach
Retention of Damp and Phlegm -- Resolve dampness and transform Phlegm basic points plus:
- SP 9 – Resolves dampness in the lower Jiao
- ST 40 – Transforms phlegm, resolves dampness, clears mind
- ST 36 – Tonifies Qi and Blood, expels wind and damp from the channels
- Ren 9 – Controls the water passages
- Ren 12 – Treats dampness, tonifies Spleen and Stomach
- Ren 17 – Regulates Qi, opens chest
Cold Accumulating in the Uterus—Warm uterus, Dispel Cold basic points plus:
- Moxa or Heat over Ren 8 (or San Jiu Jiao triangle)
- Ren 4 – Nourishes Yin and blood, Strengthens Yang, tonifies Kidney and Yuan Qi, regulates the uterus and menses
- Du 4 – Tonifies Kidney Yang, benefits Yuan Qi and Essence, expels cold from the interior of the body
- ST 36 – Tonifies Qi and blood
- BL 23 – Tonifies the Kidneys, nourishes the Essence
- BL 52 – Tonifies the Kidneys, psycho-emotional support
- BL 32 – Strengthens the lower Jiao, nourishes the Kidneys
- Shiqizhuixia – Extra point located near the 17th vertebrae (below L5), treats irregular or painful menses, and lumbar and thigh pain
Dysmenorrhea
The TCM etiology and treatment of dysmenorrhea varies according to many factors and should take into account a patient’s past and current menstrual cycles as well as other emotional and physical factors. With dysmenorrhea, there is ALWAYS pain and some form of blockage or stagnation (either qi or blood or both qi and blood). Dysmenorrhea may be caused by.... (more in course materials...)
Sample from the Chinese Medicine section of the course material:
Herbal Formula Analysis
Gui Pi Tang and Tao Hong Si Wu Tang
Gui Pi Tang is an important gynecological formula impacting the blood via its action of supplementing the Spleen qi and strengthening the Spleen function. The patient who has dream disturbed sleep, anxiety, and insomnia particularly benefits from this formula because of the mother child relationship of the Heart and Spleen and this formula’s action of nourishing the heart and tonifying the blood.
Gui Pi Tang is an excellent choice for cases of blood deficiency due to Spleen deficiency resulting in anemia and dysfunctional uterine bleeding. Often the patient will also have a weak pulse, thin pulse, pale tongue, and in some cases low grade fever or heat. When regulating the menses, it is especially helpful to have the patient take Gui Pi Tang during the post-period phase to about cycle day 14 or ovulation. The following is a breakdown of this formula and the functions of the herbs:
- Ren Shen, Radix Ginseng, 3 - 9 g. Ren Shen strongly tonifies Qi, strengthens Spleen and Lung, generates fluids, alleviates fatigue, calms the mind. Note: Ren Shen, Huang Qi, Bai Zhu, and Zhi Gan Cao are all chief herbs in this formula.
- Huang Qi, Radix Astragali Membranecei, 9 - 12 g. Huang Qi powerfully tonifies Spleen Qi, alleviates fatigue, and stops Qi deficiency bleeding.
- Bai Zhu, Radix Atractylodis Macrocephelae, 9 – 12 g. Tonifies the middle Jiao, strengthens the Spleen and dries dampness.
- Zhi Gan Cao, Radix Glycyrrhize Uralensis, 3 – 6 g. Tonifies the Spleen, tonifies Qi, and warms the middle Jiao. Gan Cao usually also harmonizes the actions of the other herbs in a formula.
- Dang Gui, Radix Angelicae Sinensis, 6 – 9 g. Dang Gui and Huang Qi work together to nourishes the blood. Dang Gui helps regulate the menstrual flow in particular. Note: Dang Gui, Long Yan Rou, Suan Zao Ren, Fu Shen, and Zhi Yuan Zhi are deputy herbs in this formula.
- Suan Zao Ren, Semen Zizyphi Spinosae, 9 – 12 g. This herb nourishes the blood, has an astringent effect on body fluids, and calms the mind.
- Long Yan Rou, Arillus Euphoriae Longanae, 6 – 9 g. Long Yan Rou has two functions in this formula: tonifies the blood and calms the mind.
- Zhi Yuan Zhi, Radix Polygalae Tenuifoliae, 3 – 6 g. This is the honey- fried preparation of Yuan Zhi. Helps the Qi flow to the Heart providing a calming an effect. This herb works especially well when balanced with Suan Zao Ren.
- Fu Shen, Sclerotium Poriae Cocos Pararadicis, 9 – 12 g. Fu Shen has a calming effect and helps support the Spleen tonics in this formula.
- Mu Xiang, Radix Aucklandiae Lappae, 3 – 6 g. This assistant herb regulates Qi, invigorates the Spleen, and prevents indigestion caused by the rick nature of the other herbs in this formula.
Traditional texts also recommend taking the formula with pieces of Da Zao (Fructus Zizyphi Jujubae) and Sheng Jiang (Rhizoma Zingiberis Officinalis Recens) to help improve the appetite and regulate the nutritive and protective Qi.