Acupuncture with physical rehabilitation improves patient outcomes for patients with infantile cerebral palsy.
Researchers from Heilongjiang University of TCM find acupuncture effective for treating infantile cerebral palsy. Combining acupuncture with physical rehabilitation increases positive patient outcomes. Cerebral palsy patients benefit from receiving both types of therapy as standalone treatment modalities but the combination protocol produces superior clinical outcomes.
Acupuncture with physical rehabilitation therapy synergistically combines to benefit infants with cerebral palsy. Based on a controlled clinical trial, researchers from Heilongjiang University of Traditional Chinese Medicine conclude that acupuncture combined plus rehabilitation is a beneficial treatment protocol for infantile cerebral palsy patients. Infantile cerebral palsy is a non-progressive condition arising from brain damage of varying causes. It may occur at any point of time before birth to one month after birth (Wang, Du and Xiong, 2011).
Major symptoms of infantile cerebral palsy include congenital motor dysfunction, abnormal posture, mental retardation, and speech impairment. Currently, patients undergo physical rehabilitation as the main form of treatment. Previous clinical research has deemed acupuncture to be influential in the treatment of infantile cerebral palsy. As a result, the researchers initiated their investigation to determine the accuracy of prior findings.
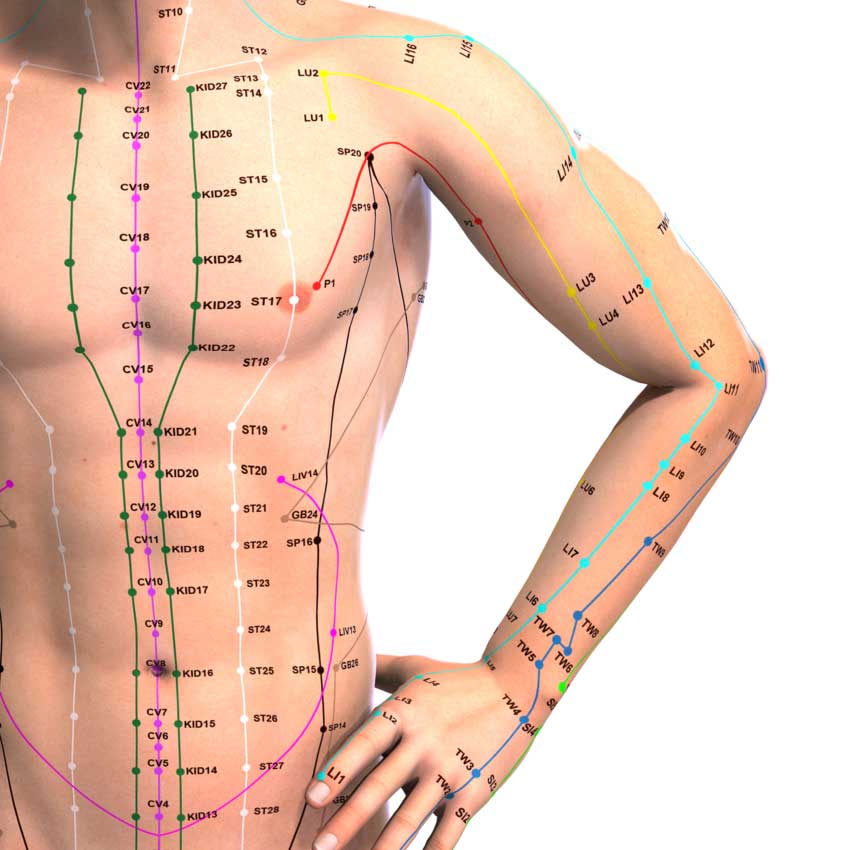
Acupuncture for infantile cerebral palsy involves scalp acupuncture and other individually determined acupoints. Scalp acupuncture dredges meridians and stimulates neural cells, which helps to restore reflex functioning. Scalp acupuncture assists in regaining limb motor functioning and improves speech abilities. Overall, acupuncture decreases the severity of cerebral palsy and improves quality of life scores. Key elements in ensuring successful outcomes are early diagnosis and treatment. Equally important, parents’ cooperation in the treatment process is needed.
The researchers from Heilongjiang University of TCM document that patients receiving combined acupuncture and rehabilitation achieved a higher Gross Motor Function Measure (GMFM) score and Barthel rating than patients who received only acupuncture treatment. Though both groups of patients responded positively to treatment, these scores indicated that the combined treatment group gained better motor functioning of the limbs and a higher ability to perform daily activities.
Fifty-four patients with infantile cerebral palsy were studied. They were equally and randomly divided into two groups: treatment group, control group. The control group received acupuncture treatment. The treatment group underwent both acupuncture and rehabilitation.
The primary acupoints selected were the same for both groups:
- Baihui (GV20)
- Qubin (GB7)
Secondary acupoints were selected on a symptomatic basis. For a weak liver and kidney:
- Taichong (LV3)
- Jiexi (ST41)
- Shenshu (BL23)
- Mingmen (GV4)
For phlegm stagnation:
- Fenglong (ST40)
- Zusanli (ST36)
- Shangjuxu (ST37)
- Geshu (BL17)
For speech impairment:
- Lianquan (CV23)
For salivation dysfunction:
- Dicang (ST4)
For a weak heart and spleen:
- Xinshu (BL15)
- Yintang (EX)
- Neiguan (PC6)
- Zusanli (ST36)
- Hegu (LI4)
- Tianshu (ST25)
- Waiguan (TB5)
For weak eyesight:
- Yangbai (GB14)
- Sibai (ST2)
For hearing impairment:
- Ermen (TB21)
- Tinghui (GB2)
- Tinggong (SI19)
- Wangu (GB12)
For the Baihui and Qubin acupoints, the Tou Ci Liu Zhen needling technique was used. A 1.5 – 2 inch (28 gauge) needle was inserted in a straight line through Baihui towards Qubin on one side of the head. The needle was inserted at 30 degrees to the scalp and constantly rotated at a speed of 200 rotations per minute for 2 minutes. Next, the process was repeated through Baihui towards Qubin on the other side of the head. A needle retention time of 50 minutes was observed. During this time, the needle was rotated once.
For the other acupoints, the Dian Ci Bu Liu Zhen needling technique was used. In this technique, a 1.5 inch (28 gauge) acupuncture needle was rapidly inserted and removed from acupoints with no needle retention time. One entire treatment cycle comprised fourteen consecutive days of acupuncture sessions. A two day break was observed before starting the next treatment cycle. A total of six treatment cycles were administered for the entire treatment course.
Head rehabilitation was executed with the help of patients’ parents. Patients received 1 of 3 different types of rehabilitation according to their individual conditions: spasms, athetosis, muscle hypotonia. For patients with spasms, a parent held the patient’s head with a palm on each side of the head. They were then instructed to pull the patient’s neck upwards. At the same time, they pressed the patient’s shoulders downwards with their forearms. For patients with athetosis, parents were instructed to straighten the patient’s arms, press downwards slightly, and turn them inwards in order to correct the outward turn. For patients with muscle hypotonia, parents were instructed to push the patient’s shoulders with their thumbs pressing against the patient’s chest, in order to help the patient lift his/her head and position it in the middle.
Sitting rehabilitation was also conducted for these 3 groups. For patients with spasms, the patient was guided to split both legs and lean forward. The trainer then straightened the patient’s lower limbs with both hands. For patients with athetosis, the trainer held the patient’s shoulders with both hands and faced it frontwards. Subsequently, the patient was guided to lift himself with his hands. For patients with muscle hypotonia, the trainer used both hands and pressed downwards on both sides of the spine with the thumb in order to straighten the patient’s head and body. When the patient’s sitting position was in order, he/she was pushed in the front, back, left and right directions to train and build his/her sense of balance.
The upper limbs and lower limbs were exercised in limb rehabilitation. For the upper limbs, the patient’s arms were lifted upwards, straightened, and turned outwards, and fingers were relaxed. If the patient’s elbow was significantly bent, it was rotated inwards before straightening the arms. Lower limbs usually suffer from stiffness and tenseness. Using the knee joints as a point of control, both legs were turned outwards to separate the legs. If the tenseness increased, hip joints were rotated and bent.
Patients’ GMFM score and Barthel ratings were recorded before and after treatment. The GMFM score was used to measure the motor function of limbs and the Barthel rating was used to measure ability to perform daily activities. The results demonstrate that acupuncture produces positive patient outcomes in the treatment of infantile cerebral palsy. However, administering it together with rehabilitation produces even greater results. The researchers conclude that pairing acupuncture with rehabilitation increases outcomes for infantile cerebral palsy patients.
References:
Li SQ. (2015). Clinical Observation on Acupuncture Combined with Rehabilitation Training for Treatment of Infantile Cerebral Palsy. Chinese Journal of Integrative Medicine on Cardio/Cerebrovascular Disease. 13(2).
Wang X, Du YH & Xiong J. (2011). Acupuncture and rehabilitation training in treating infantile cerebral palsy. 38(3): 408-413.


