Acupuncture News and Research
- Details
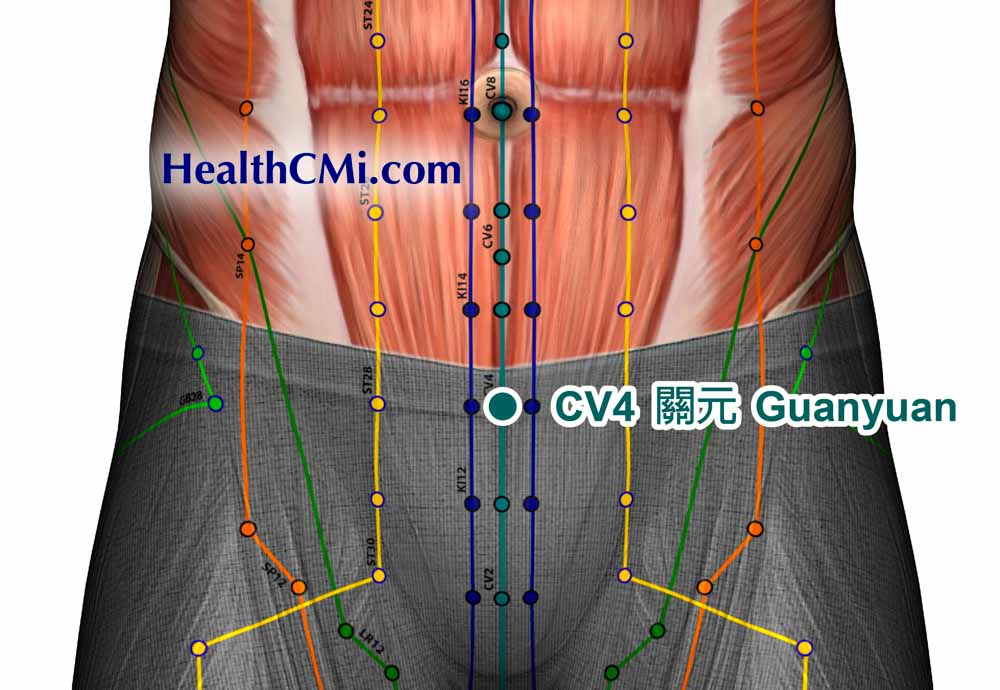
Acupuncture is effective for patients with diminished ovarian reserve (DOR) undergoing in vitro fertilization-embryo transfer (IVF-ET). In a recent clinical trial conducted by Wuhan Kangjian Maternity and Infant Hospital and the Acupuncture Research Institute of the China Academy of Chinese Medical Sciences, 80 DOR patients were recruited. The patients were randomly divided into two groups: one receiving conventional ovarian stimulation protocols and the other receiving a combination of conventional protocols and acupuncture. The results indicate that acupuncture therapy increases the antral follicle count (AFC) and improves the number of retrieved eggs, the number of high-quality embryos, and the clinical pregnancy rate in assisted reproductive cycles.
- Details
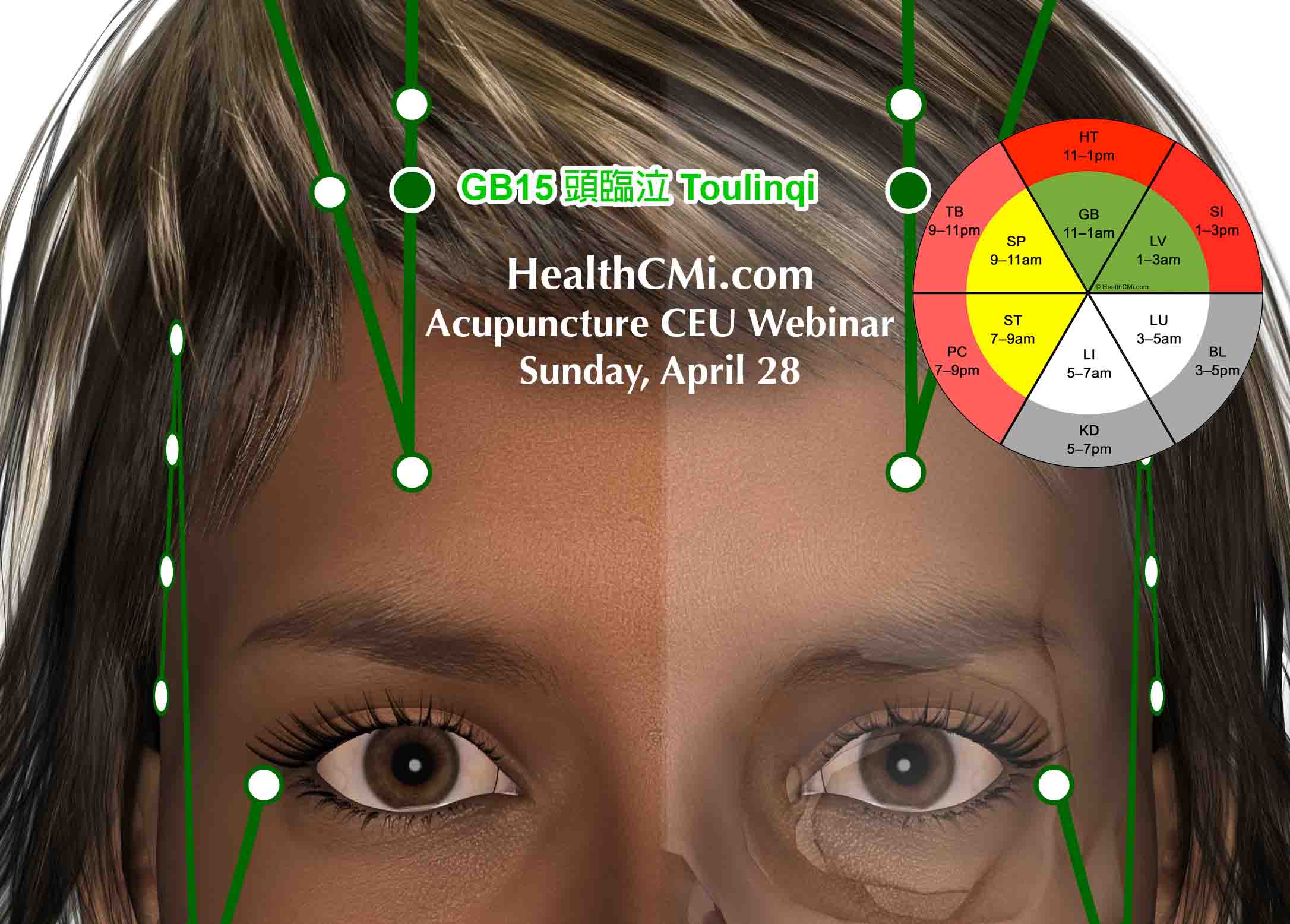
HealthCMi is airing a live acupuncture CEU webinar on the treatment of depression and neck pain. This event is Sunday, April 28th at 10 am Pacific Time. Discover how acupuncture stimulates anti-inflammatory biochemical responses to depression and pain and what endogenous biochemicals are produced in response to acupuncture needling of specific acupuncture points.
- Details

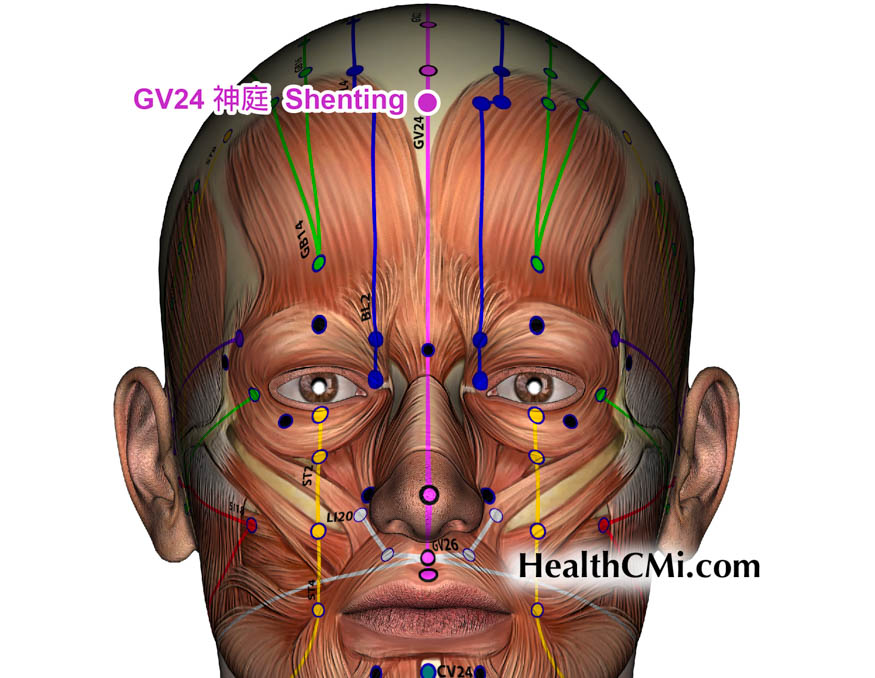
Acupuncture is effective in downregulating inflammation in patients with allergies affecting the sinuses while simultaneously alleviating symptoms. Allergic rhinitis (AR) is a common ENT (ear, nose, and throat) disorder typically characterized by a non-infectious inflammatory reaction in the nasal mucosa caused by allergens, mediated by IgE, involving multiple inflammatory factors and immune system cells. Investigators compared the efficacy of Xuanfei Tongqiao acupuncture combined with warm needle moxibustion at DU14 on patients with AR versus patients receiving the drug loratadine (an antihistamine). Acupuncture outperformed drug therapy.
- Details
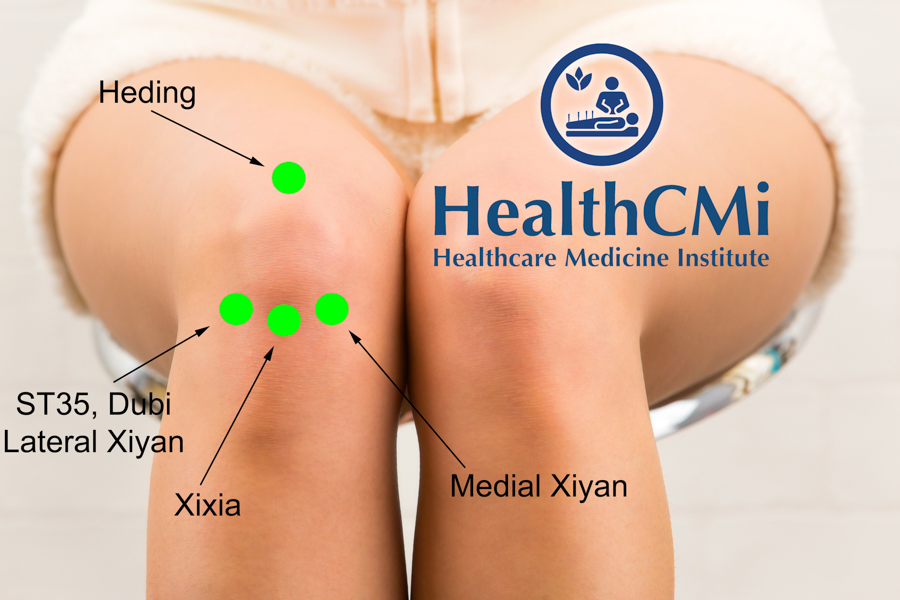
Researchers find acupuncture and herbal medicine effective for the alleviation of pain and improvement of joint function for patients with knee osteoarthritis. In an interesting result, the combination of acupuncture and herbs outperformed a powerful nonsteroidal anti-inflammatory drug (NSAID). [1] Results were based on standard Visual Analogue Scale (VAS) scores and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score.
- Details

Acupuncture is effective for the treatment of acute lumbar sprains. Researchers from the Guangdong University of Traditional Chinese Medicine and Foshan Hospital of Traditional Chinese Medicine conducted a clinical trial comparing the efficacy of routine pharmaceutical care with that of acupuncture needling with moxa and electrical stimulation. The results of the experiment indicate that the acupuncture-integrated approach yielded superior patient outcomes. [1]
- Details

HealthCMi is airing a live acupuncture CEU webinar featuring the treatment of inflammation. Groundbreaking research showing specific acupuncture points proven effective by Harvard Medical School neuroscientists is presented. Explore the anti-inflammatory acupuncture points that prevent disease progression. A special section on the treatment of uterine adhesions is presented.
- Details

HealthCMi is airing a live acupuncture CEU webinar featuring the treatment of Long COVID, wellness acupuncture visits, and pain relief. This live webinar airs on Sunday, April 7th at 10 am Pacific Time. The CEUs/PDAs count for in-person acupuncture continuing education license renewal credit. The event is acupuncture board approved. This provides CEU and PDA credit across the entire USA, plus Canada, New Zealand, Australia, and more.
- Details
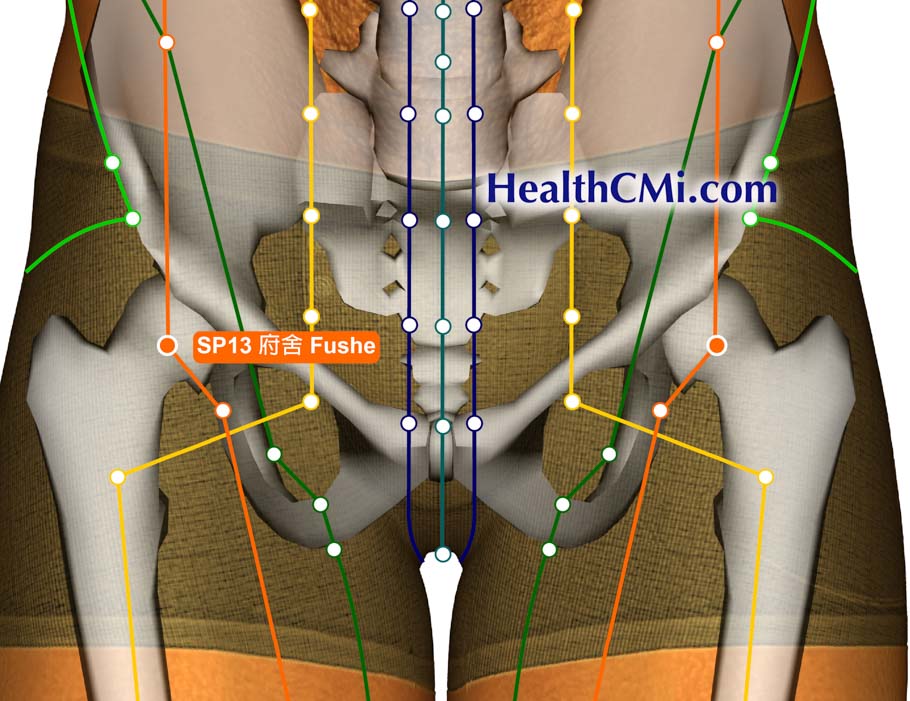
Acupuncture and Chinese herbal medicine are effective treatments for polycystic ovary syndrome (PCOS). Researchers at the Huzhou Hospital of Traditional Chinese Medicine conducted a clinical trial that compared a treatment protocol of acupuncture and usual care with a treatment protocol of acupuncture and Chinese herbal medicine for patients with PCOS. The results indicate significantly higher efficacy in the acupuncture and Chinese herbal medicine treatment group. [1]
- Details

Acupuncture is effective for the treatment of post-stroke hemiplegia. Researchers at Xinghua Traditional Chinese Medicine Hospital conducted a clinical trial to investigate the benefits of including acupuncture as supplementary therapy in the rehabilitation of stroke survivors. The results of the trial indicate that the inclusion of acupuncture significantly improved patient outcomes.
- Details
Researchers tested the efficacy of acupuncture and herbal medicine for the treatment of diabetic peripheral neuropathy. All participants in the clinical trial were provided usual care. An observation group was provided additional therapeutics with acupuncture and Chinese herbal medicine. The addition of acupuncture and herbal medicine to usual care improved overall outcomes by 7.5% and the acupuncture and herbal medicine group had significantly greater outcomes for improvements in nerve conduction velocity. [1]
- Details
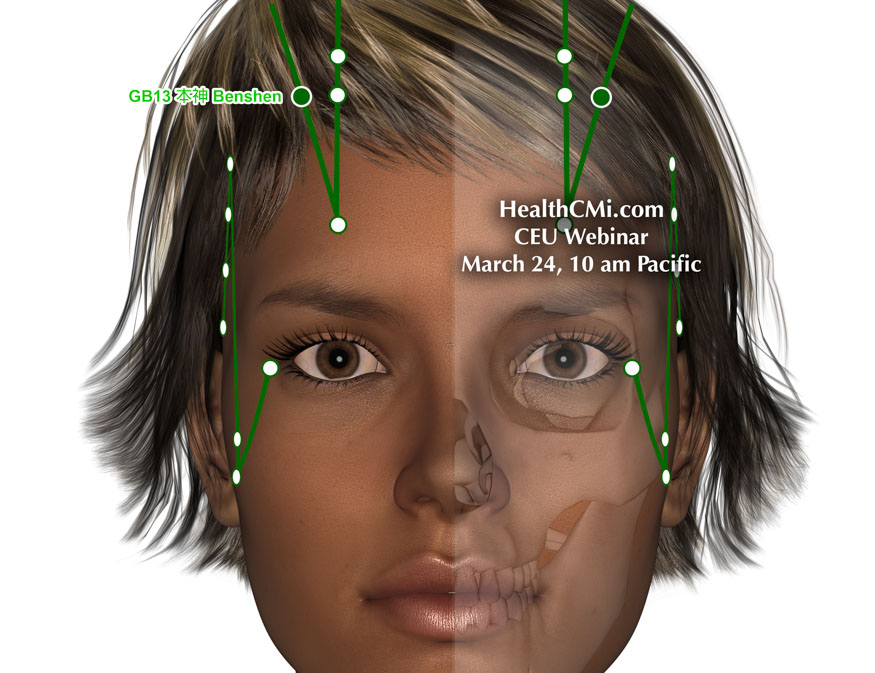
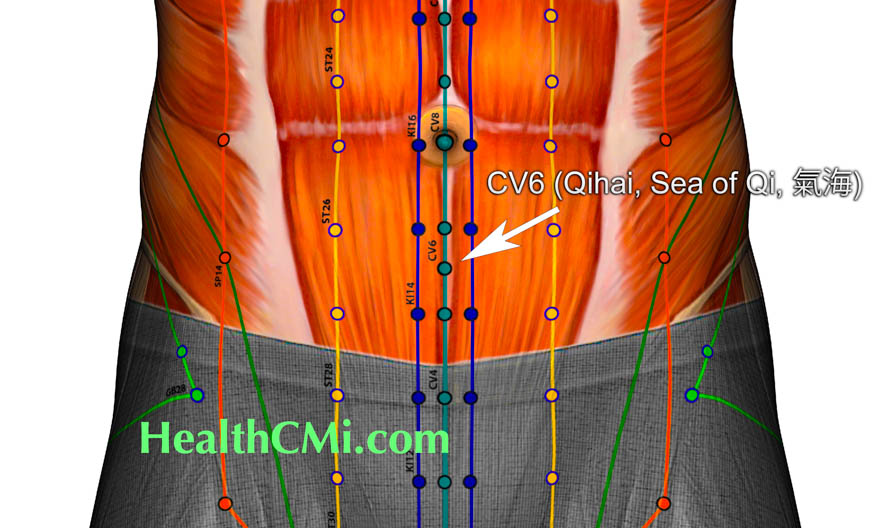
HealthCMi is airing a live acupuncture CEU webinar featuring the treatment of anxiety, hypertension, and fibromyalgia. This live webinar airs on Sunday, March 24th at 10 am Pacific Time. This webinar is acupuncture board approved for every state in the USA, including CEUs from the California Acupuncture Board, Texas State Board of Acupuncture Examiners, CTCMA (British Columbia, Canada), NZASA & Acupuncture NZ (New Zealand), NCCAOM, and many more.
- Details
Researchers find acupuncture effective for the alleviation of delayed menstruation. Two acupuncture treatments were compared, and one of the approaches to patient care produced optimal results. The researchers defined delayed menstruation as a menstrual cycle that is postponed by more than seven days (sometimes extending to 40–50 days) for two or more consecutive cycles. They classified this under the dysfunctional uterine bleeding category and add that late menstrual periods in Chinese medicine are often due to liver qi stagnation syndrome or qi and blood deficiency.
- Details

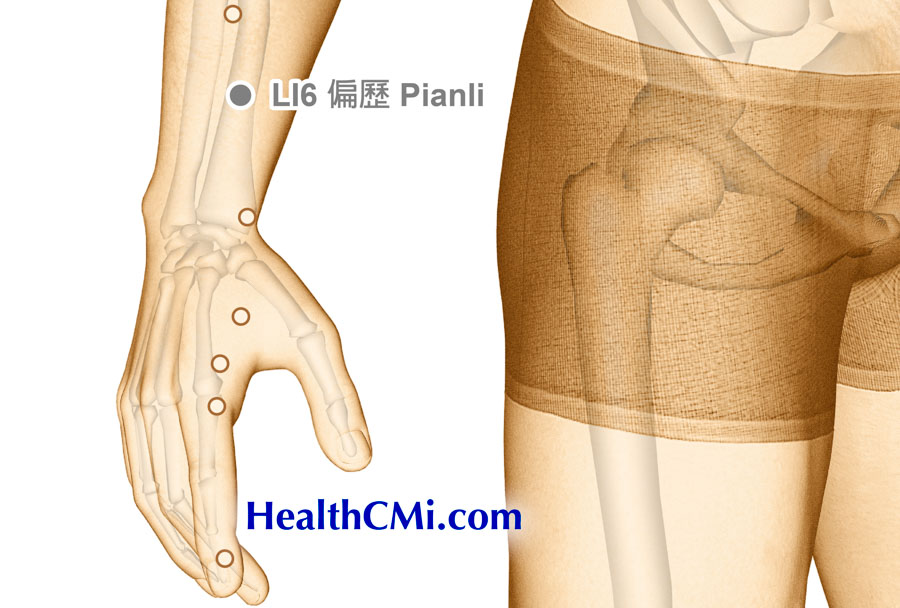
HealthCMi is airing a live acupuncture CEU webinar on the treatment of back pain and carpal tunnel syndrome. This live webinar airs on Sunday, March 17th at 10 am Pacific Time. A look at specific acupuncture points confirmed by modern research compares the efficacy of different approaches to patient care. The event covers a type of triple acupuncture that significantly promotes pain relief and recovery.
- Details

Researchers have tested and confirmed an effective acupuncture treatment for patients with functional dyspepsia (chronic upset stomach). Functional dyspepsia is characterized by a recurring upset stomach of unknown or unspecified cause. It is non-ulcerative; however, it mimics ulcerative stomach disorders. There is recurring upper abdominal pain or discomfort, often with bloating, nausea, or belching. There may be postprandial fullness or early satiation, without a clear structural cause.
- Details
Researchers find acupuncture an effective treatment modality for the alleviation of eczema (atopic dermatitis). Chronic eczema, a common dermatological condition encountered in clinical practice, presents a certain level of treatment difficulty, often accompanied by severe itching that significantly impacts patients' quality of life. The etiology of chronic eczema is complex, making the condition persistent and recurrent.
- Details

HealthCMi is airing a live acupuncture CEU webinar on the treatment of anxiety, depression, and insomnia. This special event starts Sunday, March 3rd at 10 am Pacific Time. Recent developments in acupuncture research are presented showing the relationship between medical efficacy and specific acupuncture point prescriptions. Clinical and laboratory research, along with Chinese medicine principles, demonstrate modern enhancements in patient care for optimizing results. A special focus is on moving qi circulation to enhance relaxation.
- Details

Acupuncture is effective for the treatment of PTSD, especially in combat veterans. In a high-quality placebo controlled clinical trial, researchers conclude that true acupuncture produces moderate to large beneficial clinical and biological outcomes for combat veterans with PTSD. Improvements were significant for the reduction of overall symptom severity and for large scale extinction of fear and startle responses. [1]
- Details

Acupuncture has been shown effective for the management of high blood pressure. Researchers compared the efficacy of captopril with the use of three specific acupoints. The acupoint combination outperformed the medication control group by 14%.
- Details
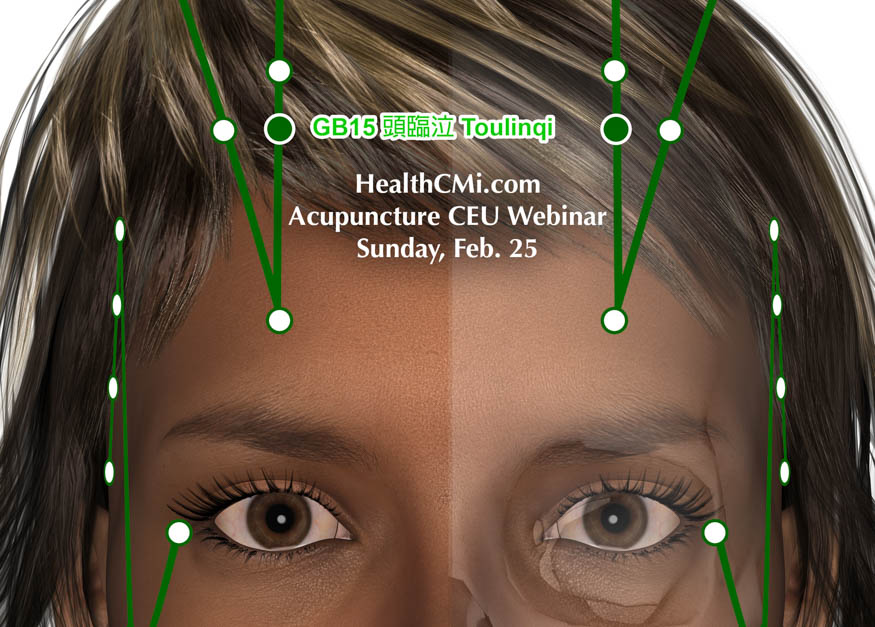
HealthCMi airs a live acupuncture CEU webinar on headache and depression relief, featuring acupuncture points proven effective in modern research. This live event is on Sunday, February 25 at 10 am Pacific Time. Participants receive full in-person acupuncture CEU credit in this online webinar. This acupuncture continuing education course is state, national, and international board approved. Explore special acupuncture points and the modern research supporting their use in clinical practice.
- Details

Acupuncture alleviates pain and motor dysfunction of the temporomandibular joint (TMJ). Researchers tested two approaches to clinical care with acupuncture. A combination of manual acupuncture plus electroacupuncture produced optimal outcomes. [1]

