Acupuncture and herbal medicine benefit patients with post-stroke aphasia. Researchers determined that patients receiving acupuncture and physical therapy combined with herbal medicine have an 11.57% increase in total efficaciousness over patients receiving only acupuncture and physical therapy. Acupuncture plus physical therapy resulted in an 86.05% total effective rate and acupuncture plus physical therapy combined with herbal medicine prodiuced a 97.62% total effective rate. [1]
Stroke patients often suffer brain damage as a result of blood vessel occlusions in the brain, leading to oxygen supply obstruction. Resultant necrosis of central nerve cells due to hypoxia-ischemia impairs local central nervous function. The brain’s language centers can easily be affected, causing impairments in listening, speaking, reading, and writing abilities—clinically referred to as aphasia. This form of cognitive impairment affects approximately a third of post-stroke patients.
Historically, acupuncture and herbal medicine have been used for post-stroke aphasia treatments for over a thousand years. Researchers decided put these time honored treatment methods into a clinical trial to determine effectiveness.
A total of 85 patients with aphasia after a stroke were selected from Xi Dian Group Hospital. Patients were given numerical orders based on the order of entry. The odd numbers were included in the control group, totaling 43 cases, and the even numbers were included in the observation group, totaling 42 cases.
Methods
Both groups received essential rehabilitation treatment and acupuncture treatment. The observation group was additionally treated with traditional Chinese herbal medicine, Di Huang Yin Zi decoction. Each patient was treated continuously for four weeks. For the control group, treatment was carried out by the same group of acupuncture practitioners. They selected several acupuncture points, using 1.5-inch stainless-steel acupuncture needles and performing regular disinfection of these points. Various techniques were used on different acupuncture points:
- Baihui GV20: Vertically pierced approximately 0.5–0.8 inches, patients experienced a sense of soreness, numbness, or pressure, then the needle was lifted and thrust at an oblique angle for tonification-sedation treatment.
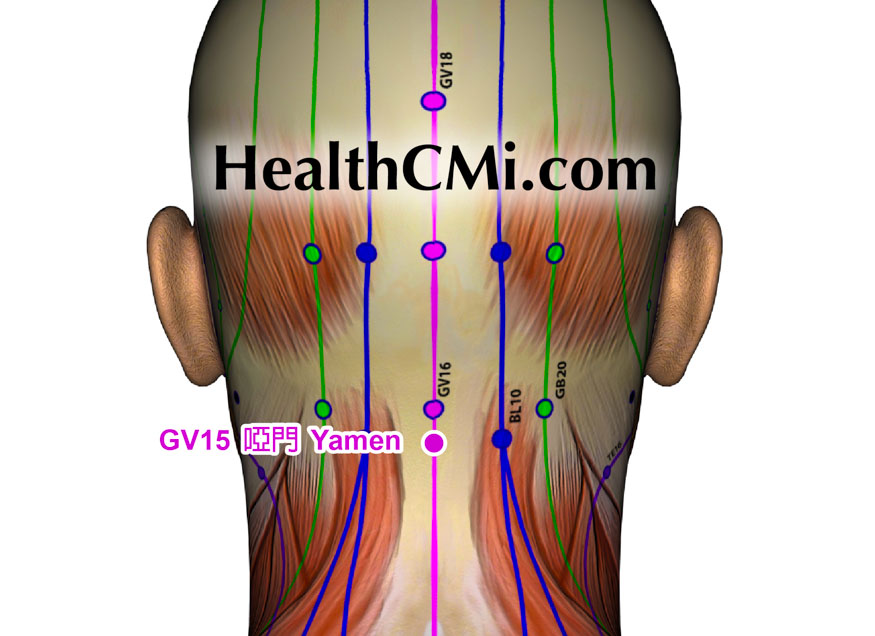
- Yamen GV15: Diagonally pierced towards the lower jaw 0.5–1 inches until patients felt the deqi sensation, then rotating the needle horizontally for tonification-sedation treatment.
- Lianquan CV23: Diagonally pierced towards the root of the tongue about 0.5–0.8 inches until patients feel the needle sensation into the root of the tongue and have a deqi, swollen feeling.
- Tongli HT5, Shenshu BL23, and Taixi KI3: Each was directly pierced by about 0.5–1 inches. After the patient felt a sense of soreness, numbness, or swelling, the needle was twisted and turned for eliciting tonification treatment.
- Sanyinjiao SP6: Directly pierced by about 1–1.5 inches, the patient felt the deqi sensation, and then the needle was lifted and thrust for tonification-sedation treatment.
All acupoints retained the needle for 30 minutes. Treatment was given once per day, and after five consecutive days of acupuncture, there was a break of 2 days. This cycle continued for four weeks in total.
In the observation group, patients were treated with the same acupuncture and physical rehabilitiation methods as the control group, supplemented by treatment with Di Huang Yin Zi Tang. The decoction's formula included Shu Di Huang, Shan Zhu Yu, Rou Cong Rong, Shi Hu, Shi Chang Pu, Yuan Zi, and Fu Ling, each 15g; Ba Ji Tian, Zhi Fu Zi, Rou Gui, Mai Dong, Wu Wei Zhi, each 10 g; fresh ginger (Sheng Jiang), 3 slices; and jujube (Da Zao), 3 pieces. The decotion was orally consumed warm in the morning and evening. One dose was given daily, and the patient continued taking it for four consecutive weeks. After four weeks of treatment, the overall efficacy rate in the observation group was 97.62%, significantly higher than the 86.05% in the control group.
Results
This study's findings indicate that compared with acupuncture and physical therapy, the combination of acupuncture and physical therapy with Di Huang Yin Zi Tang for post-stroke aphasia treatment produces optimal results. The researchers conclude that acupuncture, physical therapy, and herbal medicine in a combined treatment protocol significantly promotes patient recovery of language function and improves the clinical efficacy rate without increasing the adverse reaction rate.
Reference:
1. He Qiang, Wang Xiaorong, Zhu Jie & Lian Tengteng, 2023. Clinical efficacy and safety of acupuncture combined with traditional Chinese medicine decoction in the treatment of post-stroke aphasia. Guizhou Medicine (07), 1084-1085.


