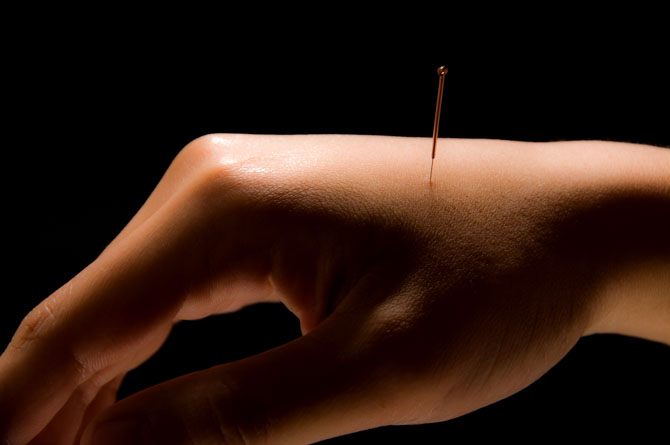
Researchers find acupuncture effective for raising positive patient outcome rates for the treatment of chronic PID.
Researchers added acupuncture and moxibustion to standard drug therapy and increased positive patient outcome rates by 35% for patients with chronic pelvic inflammatory disease. In addition, researchers combined acupuncture with herbal medicine and increased positive patient outcome rates. Based on subjective and objective findings, researchers conclude that acupuncture is an important and effective treatment modality for patients with chronic pelvic inflammatory disease (PID).

Acupuncture is effective for the treatment of PID (pelvic inflammatory disease). Zhao et al. conclude that abdominal acupuncture combined with moxibustion produces significant positive patient outcomes for patients with chronic PID. Chronic pelvic inflammatory disease (CPID) involves inflammation of female reproductive organs, surrounding connective tissues, or pelvic peritoneum. Symptoms include lower abdominal pain and leukorrhea. PID is often caused by pathogens infecting the uterus, fallopian tubes, or ovaries. Infections may involve a single organism or may be polymicrobial. Exposure to chlamydia, gonorrhea, or a history of abdominal surgery are common factors of susceptibility. Infertility due to residual scarring or congealed exudate may occur.
At the Healthcare Medicine Institute, we offer many online continuing education courses focusing on the treatment of acute and chronic PID with Chinese medicinal herbs and acupuncture. In this research by Zhao et al., CPID patients who received abdominal acupuncture and moxibustion in addition to medications reported a 100% total effective rate. The control group that received only medications reported a 65% total effective rate. The results indicate that acupuncture significantly improves the efficaciousness of drug therapy treatment.
A total of 40 CPID patients were randomly divided equally into 2 groups: treatment group, control group. Both groups received identical medications (levofloxacin lactate, metronidazole sodium chloride). After completion of menstruation, the treatment group received abdominal acupuncture and moxibustion. The primary acupoints for acupuncture therapy were as follows:
- Qihai (CV6)
- Guanyuan (CV4)
- Zhongji (CV3)
- Wushu (GB27)
- Weidao (GB28)
- Qimen (LV14)
- Zigong (EX)
Additional acupoints were selected on a symptomatic basis. For body heat and dampness:
- Sanyinjiao (SP6)
- Xuehai (SP10)
- Yinlingquan (SP9)
- Xingjian (LV2)
- Quchi (LI11)
For poor qi circulation and blood stasis:
- Hegu (LI4)
- Taichong (LV3)
- Sanyinjiao (SP6)
- Diji (SP8)
- Xuehai (SP10)
For poor qi circulation and cold stagnation:
- Zusanli (ST36)
- Xuehai (SP10)
- Ligou (LV5)
The area of treatment was first disinfected with 75% alcohol. Next, a 1.5 inch sterile disposable acupuncture needle was inserted with a high entry speed, using either the Tou Ci or Fen Ci technique. Tou Ci was performed on abdominal acupoints with the Ti Nie (pinch and lift) entry technique. For non-abdominal acupoints, Fen Ci was performed with the conventional entry technique. Upon arrival of deqi, the acupuncturist manipulated the needle with the Ping Bu Ping Xie (mild reinforcement and attenuation) technique. Subsequently, an electroacupuncture device was connected to the acupoints. An intermittent waveform was applied for abdominal acupoints and a continuous waveform was applied for the remaining points. The electrical intensity was adjusted according to the individual patient’s tolerance. Next, a needle retention time of 20 minutes was observed. Immediately after acupuncture, moxibustion was applied on acupoints selected based on individual symptoms. For stomachache, the following acupoints received moxibustion stimulation:
- Qihai (CV6)
- Guanyuan (CV4)
- Zhongji (CV3)
For lumbosacral pain, the following acupoints received moxibustion stimulation:
- Mingmen (GV4)
- Yaoyangguan (GV3)
- Yaoshu (GV2) or Yaoyan (EX)
- Baliao (BL31 – BL34)
For menopause, the following acupoints received moxibustion stimulation:
- Sanyinjiao (SP6)
For heavy menstruation, the following acupoints received moxibustion stimulation:
- Yinbai (SP1)
A moxa stick was cut into two pieces, lit, and placed in a moxa box. The moxa box was then placed on a selected acupoint. For each treatment, 2 – 4 acupoints were selected. A moxibustion session lasted 50 minutes, until the skin was flushed. Sessions were conducted once per day or every other day for 3 consecutive months. Moxibustion was not applied during menstruation. The control group and the acupuncture plus moxibustion group received identical medications. Intravenous injections were administered once daily for 3 consecutive months of the following medications:
- 0.3 g x 100 ml levofloxacin lactate injection
- 0.5 g x 100 ml metronidazole sodium chloride injection
The treatment effective rate was evaluated based on physical and gynecological examinations, and other metrics. Physical examinations measured: blood count, erythrocyte sedimentation rate, vaginal secretion, B scan, etc. Gynecological examinations measured: uterosacral ligament thickening, single or double sided oviduct, pain and surrounding masses, uterus activity, etc. On the basis of these metrics, the treatment effective rate was categorized into 4 tiers:
- Recovery: No pain in the lower abdominal and lumbosacral regions. Normal results in physical and gynecological examinations. No relapse within a month after treatment and stopping medication.
- Significantly effective: No pain or reduced pain in lower abdominal and lumbosacral regions. Improved results in physical and gynecological examinations.
- Effective: Reduced pain in the lower abdominal and lumbosacral regions. Improved results in physical and gynecological examinations.
- Ineffective: Consistent or worsened pain in the lower abdominal and lumbosacral regions. No improvement, or deterioration in physical and gynecological results.
The total treatment effective rate of 100% for the group receiving acupuncture and moxibustion in addition to drug therapy underscores the importance of accessibility to Traditional Chinese Medicine (TCM) healthcare. The control group achieved a 65% total effective rate. The results demonstrate that adding acupuncture and moxibustion to drug therapy for the treatment of chronic PID increases positive patient outcomes by 35%.
A related study finds acupuncture effective for the treatment of CPID. Song et al. (Shenzhen Longhua New District Central Hospital) determined that acupuncture produces significant increases in positive patient outcomes for patients with CPID due to qi and blood stasis. According to TCM principles, PID is due to damp-heat and toxins leading to qi and blood stasis. Biomedical pathologies associated with qi and blood stasis include pelvic masses, adhesions, and scarring.
In this study, CPID patients who received both acupuncture and herbal medicine therapy showed greater improvement than the control group, though both groups saw improvement from pre-treatment assessment. The combined treatment group reported a lower post-treatment score of 2.97 on the visual analogue scale (VAS) compared to 5.14 in the control group, reflecting a higher reduction in abdominal pain. On the McCormack scale, the combined treatment group also reported a lower post-treatment score of 4.85 compared to 7.26 in the control group.
A total of 60 patients with CPID due to qi and blood stasis participated in this study. They were randomly divided into two equal groups: treatment group, control group. Both groups received herbal medicine therapy. The treatment group received abdominal acupuncture plus herbs and the control group received only herbs. Acupoints for the treatment group were:
- Zhongwan (CV12)
- Xiawan (CV10)
- Guanyuan (CV4)
- Qihai (CV6)
- Zhongji (CV3)
- Zigong (EX)
- Wailing (ST26)
- Guilai (ST29)
- Xuehai (SP10)
- Sanyinjiao (SP6)
The patients rested in a supine position. The following protocol was applied for each acupoint. After skin disinfection, a 0.30 mm x 40 mm filiform needle was inserted into the acupoint and manipulated with the Ping Bu Ping Xie technique. Upon arrival of deqi, a needle retention time of 40 minutes was observed. One acupuncture session was conducted per day. Ingredients for the herbal medicine decoction were:
- Chi Shao (20 g)
- Dan Shen (12 g)
- Yin Chai Hu (12 g)
- Zhi Shi (10 g)
- Hong Teng (10 g)
- Fen Bao Ju (12 g)
- Yan Hu Suo (10 g)
- Tao Ren (12 g)
- Hong Hua (20 g)
- Pu Gong Ying (25 g)
- Zi Hua Di Ding (20 g)
- Yu Xing Cao (15 g)
The above ingredients were brewed in water to obtain 200 ml of concentrated herbal medicine decoction. Each decoction was split into two portions, served once in the morning and once at night. Both groups received continuous treatment over the course of three menstrual cycles. For each menstrual cycle, treatment lasted for 21 consecutive days and was paused during menstruation. Prior to and after treatment, abdominal pain was assessed according to the VAS and physical symptoms with the McCormack scale. Herbal medicine proved effective, however, the combination of acupuncture and herbal medicine produced significantly greater positive patient outcomes.
The aforementioned studies demonstrate that acupuncture increases the positive patient outcome rates for patients with chronic pelvic inflammatory disease. The first study demonstrates that drug therapy patient outcomes are greatly improved with the addition of acupuncture and moxibustion. The second study demonstrates that Chinese herbal medicine efficacy is greatly enhanced by the addition of acupuncture therapy.
References:
Zhao Y & Zhao YG. (2015). Curative Effect of Abdominal Acupuncture and Moxibustion treatment on Chronic Pelvic Inflammation. Journal of Clinical Acupuncture and Moxibustion. 31(8).
Song YJ, Zhang DQ & Su DP. (2015). Clinical Study on Abdominal Acupuncture plus Herbal Medicine for Chronic Pelvic Pain Due to Qi Stagnation and Blood Stasis. Shanghai Journal of Acupuncture and Moxibustion. 34(5).
Yang JB, Guo Y & Ni YJ. (2013). Pelvic inflammation herbal medicine and abdomen antrum transfusion in treating pelvic inflammatory diseases: 72 cases. Shaanxi Journal of Traditional Chinese Medicine. 34(9): 1165-1167.


