Researchers find acupuncture equally effective for the treatment of hypertension as the drug nifedipine, a pharmaceutical medication used for the treatment of high blood pressure and angina. Nifedipine is a calcium channel blocker that relaxes the heart muscles and blood vessels. Researchers at the Jiaozuo Tongren Hospital compared the effects of acupuncture therapy with the administration of nifedipine for the immediate reduction of high blood pressure levels in patients with primary hypertension. In the Jiaozuo Tongren Hospital randomized-controlled clinical trial, both acupuncture and nifedipine successfully reduced blood pressure by 30 – 40 mmHg. [1]
The researchers determined that acupuncture and nifedipine provided different advantages for the management of hypertension. Data points measured immediate and short-term benefits of both therapies. At the 5, 10, 15, and 20 minute data points after treatment, nifedipine produced lower systolic and diastolic blood pressures. However, at the 30 and 60 minute data points after treatment, there was no statistical difference between the effects of acupuncture and nifedipine for both systolic and diastolic blood pressure management.
Uniquely, acupuncture exerted a homeostatic regulation of blood pressure. For patients with extremely high blood pressure, acupuncture significantly reduced systolic and diastolic pressures. For patients with moderate levels of high blood pressure, acupuncture moderately reduced systolic and diastolic pressures. The clinical advantage was that acupuncture provided a regulated lowering of blood pressure relative to the clinical needs patients.
The homeostatic properties of acupuncture therapy for the treatment of hypertension indicates that acupuncture does not produce adverse hypotensive reactions. Nifedipine, by contrast, may produce excessive lowering of blood pressure, especially during the first use of the drug or if the patient is dehydrated. On balance, nifedipine has a faster effective action and acupuncture provides a more regulated reduction of blood pressure. Both therapies offer clinical advantages and provide important therapeutic choices for medical professionals.
The study design was as follows. A total of 51 patients with primary hypertension were treated and evaluated. The patients were randomly divided into an acupuncture treatment group and a drug control group, with 27 patients in the treatment group and 24 patients in the drug control group.
The statistical breakdown for each randomized group was as follows. The acupuncture group consisted of 15 males and 12 females. The age range was between 37–72 years old, with an average age of 57.39 (±13.28) years. The patients had high blood pressure with systolic blood pressure 179.97 (±11.74) mmHg or diastolic blood pressure 110.39 (±9.16) mmHg.
The drug control group consisted of 14 males and 10 females. The age range was between 36–72 years old, with an average age of 59.14 (±12.17) years. They had high blood pressure with systolic blood pressure 181.95 (±10.06) mmHg or diastolic blood pressure 109.93 (±9.79) mmHg. There were no significant statistical differences in terms of gender, age, and blood pressure measurements relevant to patient outcome measures between the acupuncture and drug groups.
The treatment group received acupuncture. Patients rested in a supine position. Acupuncture needles were applied to the following acupoints:
- LI4 (Hegu)
- LV3 (Taichong)
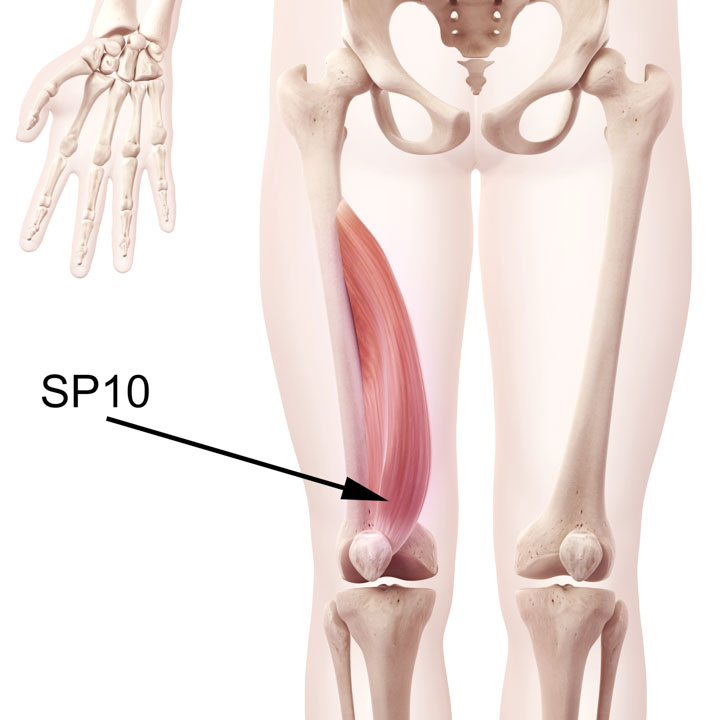
- SP10 (Xuehai)
When a deqi sensation was achieved at all acupoints, the reducing manipulation technique was applied manually. A needle retention time of 20 minutes was observed during which needles were rotated, lifted, and thrust every 5–10 minutes. The drug control group received 10 mg of nifedipine each dosage.
The acupuncture point prescription selection is supported by prior research and classical Traditional Chinese Medicine (TCM) principles. In a randomized-controlled trial, a combination of acupoints LI4, LV3, and LV2 significantly reduced blood pressure for patients with essential hypertension. In the study, acupuncture outperformed captopril, an angiotensin-converting enzyme (ACE) inhibitor, for the reduction of diastolic blood pressure. Clinical evaluations confirmed that acupuncture reduced symptoms associated with hypertension including dizziness, palpitations, and weakness. [2]
A very traditional approach to acupoint selection was used for choosing SP10 (Xuehai). According to ancient TCM principles, hypertension involves the escaping of qi and blood due to an imbalance between yin and yang. This is an historically early elucidation of the concept of homeostasis and problems arising when it is disturbed.
SP10 is renown as a Sea of Blood point and benefits patients with blood imbalances, including bleeding disorders, clotting disorders, and blood deficiency disorders. Since hypertension is related to blood circulation and SP10 treats blood imbalances, the researchers selected this acupoint. According to TCM principles, SP10 invigorates the blood and dispels blood stasis. SP10 cools the blood, benefits menstruation, and also benefits the skin. SP10 is traditionally indicated for the treatment of many disorders including irregular menstruation, painful menstruation, eczema, leukorrhea, and dysuria.
In a related study conducted at the Shanxi College of Traditional Chinese Medicine, researchers find acupuncture combined with drug therapy effective for the treatment of primary hypertension. [3] Patients were randomly and equally divided into an acupuncture treatment group and a drug group. The drug group received administration of felodipine, a calcium channel blocker used for the treatment of hypertension.
Acupuncture plus felodipine produced an 86.7% total effective rate. Using only felodipine, the total effective rate was 73.3%. The researchers note that the integrative medicine approach to the treatment of hypertension improves patient outcomes by 13.4%.
The researchers discovered that both acupuncture and felodipine regulated E-selectin, iNOS, and eNOS expression to normal levels. The restoration to normal levels of E-selectin, iNOS, and eNOS expression was directly correlated with normalization of blood pressure levels. The study indicates that regulation of E-selectin, iNOS, and eNOS demonstrates one mechanism of effective action of acupuncture for the treatment of hypertension. Further, the researchers note that the anti-hypertensive action of acupuncture “relies on the improvements in vascular endothelial cellular function” related to the regulation of E-selectin, iNOS, and eNOS. [4]
This conclusion is supported by additional research finding that “In the blood vessel wall, NO [nitric oxide] is produced mainly from l-arginine by the enzyme endothelial nitric oxide synthase (eNOS)…. Dysfunction in the production and/or the bioavailability of NO characterizes endothelial dysfunction, which is associated with cardiovascular diseases such as hypertension and atherosclerosis.” [5]
E-selectin is involved in the regulation of inflammation. It is a molecule expressed on endothelial cells that is activated by cytokines. Inducible nitric oxide synthase (iNOS) is an enzyme that generates nitric oxide (NO) from l-arginine (an amino acid). iNOS is an important enzyme involved in blood pressure regulation and inflammation. [6] Endothelial NOS (eNOS, nitric acid synthase) is an enzyme that synthesizes nitric oxide and is involved in inflammation and cardiovascular function.
Researchers find both acupuncture and drugs effective for the management of hypertension. One advantage of acupuncture therapy is that it produces minimal adverse effects, especially when compared with medications. Medications have an important advantage. They are easily accessible and are often affordable. Researchers also find that acupuncture combined with medications produces optimal patient outcomes. This brings to light the importance of patient accessibility to treatment options for the regulation of hypertension.
To learn more, listen to the podcast:
References
1. Liu XS. Observation on the Immediate Buck Effect of the Siguan and Xuehai Points Needling [J]. Clinical Journal of Chinese Medicine, 2014(4):61—63.
2. Xie, B., and Y. P. Lin. "Efficacy observation on acupuncture for essential hypertension of yin deficiency due to yang hyperactivity pattern." Zhongguo zhen jiu= Chinese acupuncture & moxibustion 34, no. 6 (2014): 547-550.
3. Chen J, Li J, Wang ZR. Therapeutic Effect on Essential Hypertension Treated with Combined Therapy of Acupuncture and Medication [J]. Chinese Acupuncture & Moxibustion, 2010, 30(11):896—898.
4. Chen J, Li J, Wang ZR. Therapeutic Effect on Essential Hypertension Treated with Combined Therapy of Acupuncture and Medication [J]. 2010, 30(11):896—898.
5. Zhao, Yingzi, Paul M. Vanhoutte, and Susan WS Leung. "Vascular nitric oxide: Beyond eNOS." Journal of pharmacological sciences 129, no. 2 (2015): 83-94.
6. Lechner, Matthias, Philipp Lirk, and Josef Rieder. "Inducible nitric oxide synthase (iNOS) in tumor biology: the two sides of the same coin." In Seminars in cancer biology, vol. 15, no. 4, pp. 277-289. Academic Press, 2005.


