Acupuncture outperforms drug therapy for the treatment of mild to moderate female stress urinary incontinence (FSUI). Researchers from Weihai City Hospital of Traditional Chinese Medicine conclude that electroacupuncture is effective for the control of FSUI. In the study, an electroacupuncture treatment group produced a positive patient outcome rate of 86.7%. The drug control group produced a 68.9% positive patient outcome rate for the treatment of FSUI. The electroacupuncture group had a significantly higher complete recovery rate and total effective rate.
After four weeks of treatment, the electroacupuncture group achieved a positive patient outcome rate of 86.7%. A total of 30 patients fully recovered, 48 showed significant improvements, and 12 had no improvements. The drug control group had a 68.9% positive patient outcome rate. A total of 20 patients fully recovered, 42 showed significant improvement, and 27 had no improvements. The positive patient outcome rates show significant differences between these treatment protocols.
Patients in the drug control group received administration of midodrine hydrochloride. The researchers chose midodrine, an adrenergic agent and alpha-stimulant, because urodynamic measurements find it effective for increasing maximum urethral closing pressure (Garofalo et al.). Based on the findings of the controlled investigation, the researchers conclude that electroacupuncture outperforms midodrine hydrochloride for the treatment of FSUI. In addition, the researchers note that electroacupuncture is both safe and effective for the treatment of mild to moderate level FSUI, producing no serious adverse effects.
Female stress urinary incontinence is characterized by the involuntary loss of urine control. Leakage typically occurs during activities that cause changes in abdominal pressure, including coughing, laughing, and positional changes. Any movements (including standing, sitting, or movement during sleep) may may trigger the involuntary loss of urine. In severe cases of FSUI, women may require the use of a pad. For the purposes of this study, only mild to moderate FSUI was investigated. Patients with severe FSUI were not included in this study.
The study design was as follows. A total of 180 patients were randomly distributed into a control group and a treatment group, each consisting of 90 cases. The control group received standard drug therapy. The treatment group received electroacupuncture. All patients were diagnosed with female stress urinary incontinence between April 2013 and May 2015.
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 46 mild cases and 44 moderate cases. The average age in the treatment group was 52 (±9) years. The average course of disease in the treatment group was 15.3 (±7.0) months.
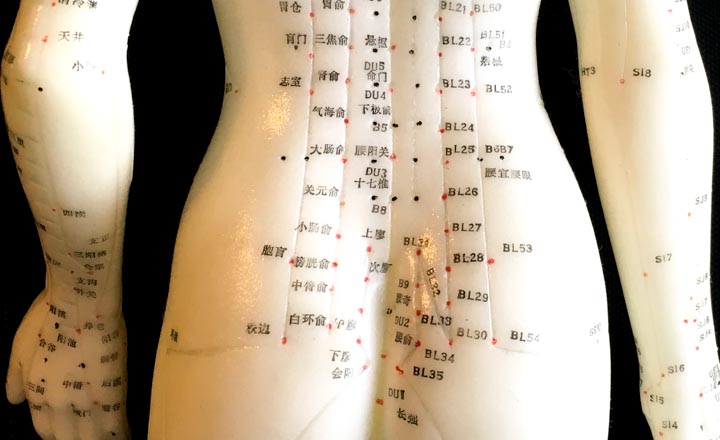
The control group was comprised of 48 mild cases and 42 moderate cases. The average age in the control group was 51 (±8) years. The average course of disease in the control group was 14.9 (±7.2) months. There were no significant statistical differences in terms of age, course of disease, and severity of disease between the two groups. For the treatment group, the following protocol was administered. Upon disinfection with 75% ethanol, a 0.35 mm × 50 mm filiform acupuncture needle was inserted into the following acupoints:
- BL32 (Ciliao)
- BL23 (Shenshu)
- BL35 (Huiyang)
BL23, BL32, and BL35 are all located on the bladder meridian of foot Taiyang. Wang et al. note that “these three acupoints are combined to warm the kidneys, strengthen the spleen, restore yang qi, so that the normal function of the kidney and bladder can be recovered and incontinence can be relieved.” Once manual acupuncture elicited an electric shooting sensation radiating toward the perineum and urethra, electroacupuncture was applied. A disperse-dense wave of 50 – 70 Hz was applied with an intensity level set to patient tolerance levels or until perception of an electric sensation. Electroacupuncture was applied once per day, 30 minutes per acupuncture session, 6 times per week, for a total of 4 weeks.
The researchers note that “electroacupuncture not only activates meridian qi, but also improves functions of nerves and muscles.” BL32 acts on the posterior branch of the sacral nerve. BL23 acts on the lateral division of the posterior branch of the first lumbar nerve and the first major branch of the lumbar plexus. BL35 acts on the sacral plexus. When these acupoints and their relevant nerves were stimulated with electroacupuncture, the pelvic floor muscles are passively exercised to improve the local blood circulation and to control incontinence.
The control group received midodrine hydrochloride. Midodrine is an alpha-1 adrenalin receptor agonist, which may be used for the treatment of urinary incontinence. It selectively stimulates alpha-1 adrenalin receptors, leading to smooth muscle contraction of the urinary tract. The potential side effects of the drug includes hypertension, paraesthesia and itchiness of skin, and shivers. A total of 2.5 mg of midodrine hydrochloride tablets were orally administered three times per day, for a total of 4 weeks.
Patients were evaluated before and after the treatment course. Severity of incontinence was evaluated based on the International Consultation on Incontinence Questionnaire-Short Form (ICI-Q-SF). This is a subjective measure of severity of urinary loss and quality of life. A one hour pad test was also conducted to confirm results with objective measures. The treatment efficacy for each patient was evaluated and categorized into 1 of 3 tiers:
- Recovery: Complete elimination of symptoms. 100% improvement in ICI-Q-SF score. Negative results of one-hour pad test.
- Effective: Significant absence of symptoms. 30% –99% improvement in ICI-Q-SF score. Positive results of one-hour pad test.
- Not effective: Symptoms showed no visible improvement. <30% improvement in ICI-Q-SF score. Positive results of one-hour pad test.
Acupuncture produced a higher total effective rate and higher total recovery rate than drug therapy. The findings indicate that integration of acupuncture into usual care protocols is warranted. Traditional Chinese Medicine (TCM) has a long history concerning the treatment of urinary incontinence. Now, modern scientific data confirms the efficacy of acupuncture for the treatment of urinary incontinence with both subjective and objective data.
References
Wang et al. Observations on the Therapeutic Effect of Electroacupuncture on Mild and Moderate Female Stress Incontinence [J]. Shanghai Journal of Acupuncture and Moxibustion, 2016(1):47–49.
Garofalo, F., G. M. Lalanne, and G. Nanni. "Midodrine for female incontinence: a preliminary report." Clinical therapeutics 9, no. 1 (1985): 44-46.


