 Photograph: HealthCMi, Adobe Images
Photograph: HealthCMi, Adobe Images
Researchers investigated the effects of acupuncture combined with joint mobilization on patients with ankle dysfunction. The researchers conclude that acupuncture combined with joint mobilization produces a 59.65% total effective rate. Ankle dysfunction often occurs as a result of acute ankle sprains, ankle fractures, or due to complications following ankle surgery. Ankle sprains cause damage to the medial or lateral ligaments, which leads to pain and swelling. Some patients are unable to fully recover, affecting their ankle motor functions and increasing the tendency for another sprain. Complications due to surgery and untreated ankles may lead to valgus or an unsteady gait; severe consequences include joint deformity or traumatic arthritis. Also, some patients may experience ankle pain, movement dysfunction, or ankylosis (Zhou et al.).
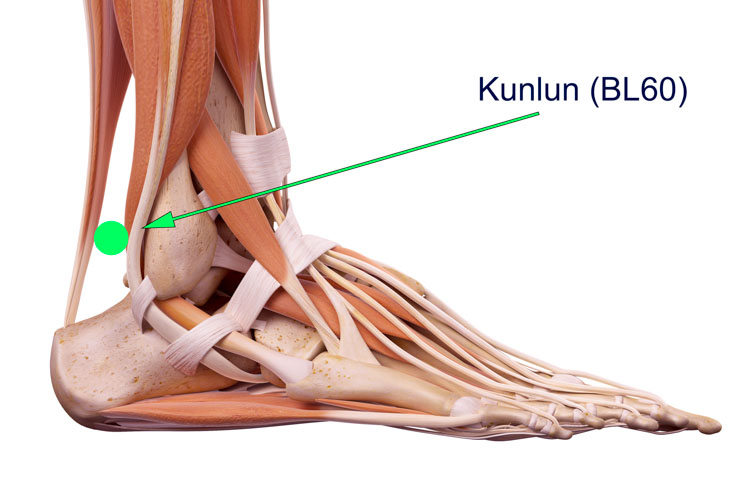
Ankle dysfunction is mainly caused by tendon or joint injuries; ankle sprains lead to blood stasis, poor blood and qi circulation, and blocked meridians that induce pain. In Traditional Chinese Medicine, ankle dysfunction is in the scope of tendon and muscle injuries (Jin Shang). Acupuncture and moxibustion improve the Yin and Yang balance (Zhang). For ankle dysfunction, common acupoints treated include Shenmai, Zhaohai, Jiexi, Taixi, Kunlun, Yanglingquan, and localized Ashi acupoints. The Taixi (KD3) acupoint is the primary-yuan acupoint on the Kidney Meridian (Foot Shao Yin); this acupoint is traditionally indicated for treating ankle pain. The Jiexi (ST41) acupoint is located on the Leg Yang Ming Stomach Meridian; this acupoint is useful in dredging meridians and promoting the health of joints, the spleen, and the stomach, as well as promoting qi and blood circulation.
The Kunlun (BL60) acupoint is located on the Bladder Channel of Foot Tai Yang; this acupoint helps remove blood stasis, relieves swelling, warm the meridian, expel chills, and promote blood circulation. The Yanglingquan (GB34) acupoint is excellent in treating all diseases related to tendon injuries. The Shenmai (BL62) acupoint is located on the Bladder Channel of Foot Tai Yang. It is also the first acupoint on the Yang Heel Vessel, and this acupoint can be used to treat pronation disorders. The Zhaohai (KD6) acupoint is located on the Kidney Meridian (Foot Shao Yin). It is also the first acupoint on the Yin Heel Vessel, and this acupoint can be used to treat inversion of the foot. The details about treatment methods are as follows:
Acupoints treated include Shenmai (BL62), Zhaohai (KD6), Jiexi (ST41), Taixi (KD3), Kunlun (BL60), Yanglingquan (GB34), and localized Ashi acupoints. Upon disinfection, acupuncture needles (gauge #28, 35 mm length, hao type) were inserted. During each acupuncture session, 3 to 5 acupoints were selected for insertion. Acupuncture needle manipulation techniques used were rotating and reducing (xie) methods. The acupuncture needles were manipulated every 5 to 10 minutes. The needle retention time was 30 minutes. If there was no obvious swelling or the course of disease was more than 10 days, the acupuncture therapy continued without change. If there was significant swelling, pyonex tapping needles were used to release blood stasis, followed by cupping to facilitate removal of blood stasis; this treatment was conducted every other day.
The breakdown of traditional acupoint indications, functions, and channel theory is included in the research analysis. This approach extends acupuncture continuing education throughout the discussion portion of the research article and is consistent with modern standards of reporting. Prevalent across many educational acupuncture investigations is the inclusion of Traditional Chinese Medicine (TCM) theory combined with modern biomedical and scientific data. Medicine is presented in the form of an uninterrupted timeline, wherein ancient principles and modern findings are complementary and serve to shed the light of greater understanding on treatment options and patient outcomes. The polarization of medicine into Eastern and Western schools of thought, or old versus new, falls by the wayside as modern research finds consistency and correlations between varying evolutions in philosophies of medicine.
Specific treatment modalities, often perceived as either traditional, Asian, Western, etc… are in reality ubiquitous both geologically and historically. In this research, arthrolysis joint mobilization (mobility restoration by disruption of adhesions in ankylosed joints) was combined with acupuncture into a comprehensive protocol. The combination of acupuncture and arthrolysis may be seen as a new combination; however, for well over 1,000 years, tui-na bodywork techniques have been incorporated into the canon of Traditional Chinese Medicine. Tui-na encompasses what is understood in the occident as osteopathy, chiropractic manipulations, orthopedics, massage therapy, arthrolysis, and physical therapy. One of the earliest introductions to physical medicine in the form of tui-na was in the Huangdi Neijing (The Yellow Emperor’s Classic of Medicine).
Many scholars document that the great classic text, the Huangdi Neijing, was written circa 300 BCE, although some historical approximations suggest that early forms of the text may date as far back as 2,600 BCE. The exact date of specific sections may vary and is the subject of a great many acupuncture continuing education investigations. That said, many scholars suggest that the Huangdi Neijing may be a compilation, which explains variations on the exact date of authorship. In the text, tui-na is cited as having the ability to promote qi and blood circulation, benefit muscles and tendons, clear the channels and collaterals, and more. Based on a historical perspective, the combination of acupuncture and arthrolysis is a time honored tradition. This research formalizes and tests that long-standing combination.
For the duration of acupuncture therapy, patients were asked to minimize movements of the affected limb (especially the activities of standing and walking for an extended period) as well as moderating rigorous sports activity. When at rest, the patients were instructed to raise the affected limb. Keeping the affected limb warm during cold weather was also important to prevent the disease from becoming chronic or worsening. Acupuncture and arthrolysis therapy was conducted on a daily basis, and one course of treatment lasted for 10 days. Four arthrolysis techniques were applied in addition to acupuncture therapy.
- Technique 1: The patient’s affected limb was bent at 90 degrees. The doctor held the patient’s affected medial and lateral malleolus with both hands. The doctor’s hand moved upward with force to create separation traction.
- Technique 2: The patient’s affected limb was bent at 90 degrees. The doctor’s right hand was placed in front of the patient’s talus; the left hand was fixated behind the ankle. The right hand pushed the talus posteriorly. Subsequently, the doctor’s left hand was placed behind the patient’s talus; the right hand was placed in front of the patient’s talus. The left hand pushed the talus toward anteriorly, medially, and laterally to obtain a sliding motion of the talus.
- Technique 3: The patient was asked to rest in a prone position, his/her affected limb was stretched straight, and the ankle should was suspended in the air while the patient rested on the bed. The doctor’s left hand held the ankle from behind; the right hand held the calcaneus and talus. The right hand pushed the calcaneus and talus medially and laterally.
- Technique 4: The patient was asked to rest in a supine position. The doctor’s left hand held the patient’s heel from behind; the right hand held the front of the heel. Both hands rotated the heel medially and laterally.
Each of the above techniques were repeated 3 to 4 times; the total treatment time was 15 to 20 minutes per arthrolysis session. Based on the patient’s pain tolerance levels, arthrolysis was conducted once per day or every other day, for 10 days, to complete one course of treatment. The researchers conclude that acupuncture combined with joint mobilization therapy (arthrolysis) produces a 59.65% total effective rate for the treatment of ankle dysfunction.
References
Chen X., Mu J.P., Peng L., Liao H., Zhang Q. (2013). Acupuncture Combined with Joint Mobilization for the Treatment of Ankle Dysfunction. JCAM. 29(10).
Zhang W. (2012). Acupuncture, moxibustion, and physiotherapy in treating ankle sprain. Journal of Traditional Chinese Medicine. (7): 113.
Zhou S., Zhao P.F., Liu Y.X., et al. (2003). Analysis on the causes of ankle dysfunction as a result of ankle fracture. Chinese Journal of Orthopedics and Traumatology. 11(5): 34.


