Acupuncture alleviates dementia and cognitive impairment. Researchers from the Anhui University of Chinese Medicine demonstrate that acupuncture has a 90% total effective rate for the treatment of vascular dementia. Researchers from the Heilongjiang University of TCM (Traditional Chinese Medicine) demonstrate that acupuncture improves cognitive abilities for patients with non-dementia related vascular cognitive impairment. In addition, researchers from the Tianjin University of Traditional Chinese Medicine demonstrate that acupuncture has an 88% total effective rate for the treatment of chronic cerebral circulatory insufficiency (CCCI). 
The studies demonstrate that acupuncture benefits patients with disorders linked to impairment of blood flow to the brain. Vascular dementia involves difficulty with reasoning, memory, and thinking. Vascular cognitive impairment with no dementia (VCIND) is prodromal dementia characterized by mild cognitive impairment (MCI). Chronic cerebral circulatory insufficiency is cerebral vascular insufficiency often caused by atherosclerosis or a stroke. Dizziness, tinnitus, blurry vision, depression, confusion, memory loss, and general senility are common characteristics of this disorder.
The Anhui University of Chinese Medicine researchers randomly divided sixty vascular dementia patients into two groups. Group one received scalp acupuncture with a long needle retention time. Group two received thirty minute acupuncture sessions. The group with the long scalp acupoint needle retention times demonstrated a 90% total effective rate. The group receiving acupuncture with thirty minute needle retention times achieved a 66.7% total effective rate.
Group one received scalp acupuncture at the following acupoints:
- Baihui, DU20
- Sishencong (extra point set)
- Shenting, DU24
DU24 and Sishencong were needled towards DU20. Manual acupuncture needle stimulation, including rotation, was applied to each needle. The acupuncture needles at the scalp acupoints were retained for eight hours.
Supplementary acupoints included Fengchi (GB20), Yintang, Zusanli (ST36), and Taixi (KD3). Additional acupoints were added based on differential diagnostics. For liver and kidney deficiency, Ganshu (BL18) and Shenshu (BL23) were applied. For phlegm stagnation, Fenglong (ST40) and Zhongwan (CV12) were added. For blood stasis and meridian blockage, Xuehai (SP10) and Geshu (BL17) were added.
ST36 and KD3 were applied with tonification manual acupuncture techniques. The other supplemental points were applied with mild reinforcing and reducing techniques. Total needle retention time for supplemental acupoints was thirty minutes per acupuncture session. Manual stimulation was applied once every ten minutes during each session. Acupuncture was administered once per day for five contiguous days followed by a two day break from treatment. The total treatment period was eight weeks comprised of eight courses of acupuncture care.
Group two received nearly identical treatments as group one. However, total needle retention time for all needles was thirty minutes. Scalp acupuncture points were not retained over a long duration as in group one.
Several methods and indexes were used to evaluate cognitive abilities. The Mini Mental State Examination (MMSE) and the Blessed Dementia Scale (BLS-D) measured changes in orientation, calculation, memory, and articulation. Ability to conduct activities of daily living were based on the Barthel Index (BI). This measured abilities concerning food ingestion, bodily motions, walking, showering, urination, and defecation. 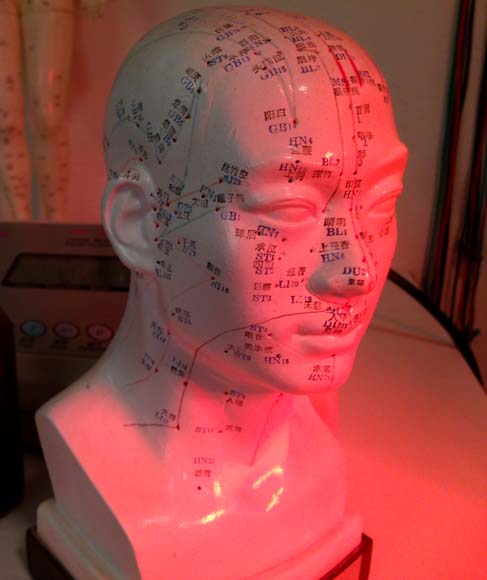
The long needle retention times of scalp acupuncture points yielded significantly greater positive patient outcomes. A 90% total effective rate in group one over the 66.7% total effective rate in group two demonstrates vast differences in clinical results. The researchers note that longer acupuncture needle retention times more effectively stimulate meridian Qi, which dredges the meridians.
In related research, Tianjin University of Traditional Chinese Medicine researchers compared acupuncture with nimdopine for the treatment of chronic cerebral circulatory insufficiency (CCCI). Nimodipine, a calcium channel blocking agent, is used for the treatment of disorders due to the lack of brain oxygen caused by bleeding from a blood vessel in the brain. Nimodipine is used for the prevention of cerebral vasospasms and associated ischemia.
Acupuncture achieved an 88% total effective rate. Nimodipine achieved a 76% total effective rate. The Tianjin University of Traditional Chinese Medicine researchers note that these findings are consistent with that of Wang et al. In the publication of their research entitled Research on Acupuncture Therapy in Treating Ischemic Cerebrovascular Disease and its Effects on Brain Blood Flow, Wang et al. note that acupuncture increases regional brain blood flow and supply. In addition, acupuncture improves lipid metabolism and blood clot removal.
The Tianjin University of Traditional Chinese Medicine researchers document that acupuncture increases blood flow velocity (MCA, PCA, VA, BA, etc…) and is more effective than nimodipine. Clinical improvements included reduction of headaches, dizziness, insomnia, and depression. Acupuncture points used in the study included:
- Fuliu, KD7
- Shangxing, DU23
- Yintang
- Wangu, GB12
- Fengchi, GB20
- Quchi, LI11
- Shousanli, LI10
- Lieque, LU7
- Hegu, LI4
- Xuehai, SP10
- Zusanli, ST36
- Fenglong, ST40
- Taichong, LV3
Researchers from Heilongjiang University of TCM conducted research to study the efficacy of acupuncture combined with cognition training rehabilitation on non-dementia vascular cognitive impairment (VCIND). A group receiving both cognition training and acupuncture had significantly greater positive patient outcomes than a group receiving only cognition training. The results demonstrate that acupuncture is effective as part of a comprehensive therapeutic approach for the treatment of VCIND.
The scalp acupuncture techniques used in the research involved needle retention times of six hours per acupuncture session. In addition, disperse-dense wave electroacupuncture was applied to the scalp acupuncture points. The effectiveness of long needle retention times for scalp acupuncture points is consistent with the findings of the Anhui University of Chinese Medicine researchers. In addition, the research consistently demonstrates that acupuncture is an effective treatment for dementia and cognitive impairment.
References:
Wang Y, Zhu CQ & Chen SF. (2014). Clinical Effect of Long-Term Scalp Acupuncture in Treatment of Vascular Dementia:A Report of 30 Cases. Journal of Anhui Traditional Chinese Medical College. 33(2).
Qu YJ, Zhuo L & Wang HL et al. (2013). 1980-2011 China community vascular dementia meta-analysis of 55 years old and above patients. Chinese Journal of Stroke. 8(7): 533-543.
Luo, X. H., Sun, L. & Wu, J. (2014). Clinically Therapeutic Research on CCCI Patients by Acupuncture Therapy of Shengqing Jiangzhuo. Journal of Clinical Acupuncture and Moxibustion. 30(10).
Peng, J. D. (2011). Scientific Interpretation by Professor Wu Lian Zhong. Journal of China Acupuncture. (7): 631-634.
Sun, C. X. (2002). Clinical Diseases Diagnosis and Treatment Effectiveness Standard. Beijing: People’s Medicine Publisher. 511.
Wang, F. & Jia, S. W. (2001). Research on Acupuncture Therapy in Treating Ischemic Cerebrovascular Disease and its Effects on Brain Blood Flow. Journal of China Acupuncture. (4): 58-60.
Zhang L, Liu SX, Xing YL, Wang Y & Guan Y. (2014). Efficacy of Acupuncture Combined with Rehabilitation on Non Dementia Vascular Cognitive Impairment. Journal of Clinical Acupuncture and Moxibustion. 30(12).
Hachinski VC, Bowler JV. Vascular Dementia. Neurology, 1993, 43(10): 2159 – 2160.
Rockwood K. Vascular cognitive impairment and vascular dementia. Neurology, 2002, 15(203-204): 23-27.


