Acupuncture alleviates cerebral palsy related hearing disorders and excess drooling.
Hospital researchers find acupuncture effective for relieving excessive drooling and for improving hearing in cerebral palsy patients. In a surprise finding, the optimal acupuncture needle retention time for benefitting hearing was not the longest retention time. A shorter duration produced superior patient outcomes. Take a look at the findings and protocols to learn what the researchers discovered.

Acupuncture is an effective treatment for cerebral palsy related complications, including drooling and hearing disorders. In a clinical study conducted at Neijiang Second People’s Hospital, researchers Xie and Lu determined that acupuncture and massotherapy significantly alleviate drooling and improve quality of life scores for cerebral palsy patients. Evidence suggests that cerebral palsy (CP) related drooling is correlated with motor impairments affecting swallowing (Senner et al.). This condition affects the overall quality of life and may impede speech and increase risk of infectious diseases.
Xie and Lu conclude that cerebral palsy patients treated with acupuncture and massotherapy had significantly greater positive patient outcomes than patients in the control group that did not receive either acupuncture or massotherapy. Patients receiving acupuncture with massotherapy demonstrated less drooling and significant improvements in fine motor movements, adaptive behavior, and social behavior over the control group. Acupuncture plus massotherapy patients also demonstrated the ability to take meals independently more significantly than the control group.
For the study, 48 patients with cerebral palsy related drooling were treated. They were equally divided into two groups: treatment group, control group. Patients in the control group carried out strengthening exercises for the mouth and received external application of Chinese herbs on selected acupoints. Patients in the treatment group received the same therapy with additional acupuncture and massotherapy treatments. For all therapies conducted, one entire treatment course comprised 10 consecutive days. The primary acupoints selected for acupuncture in the treatment group included the following:
- Lianquan (CV23)
- Dicang (ST4)
- Jiache (ST6)
- Xiaguan (ST7)
Secondary acupoints included the following:
- Baihui (GV20)
- Shangxing (GV23)
Strong stimulation was applied to the Lianquan (CV23) acupoint by inserting a standard acupuncture needle into the root of the tongue in a slanted orientation to a depth of 0.5 to 0.8 inches. The needle was then rotated at high speed for 20 to 30 seconds until the patient felt soreness, numbness, and a sensation of heaviness at the root of the tongue. Once the patient felt these sensations, the needle was removed immediately, with no needle retention time.
For the Xiaguan (ST7) acupoint, the needle was inserted vertically to a depth of 0.5 inches. For the Dicang (ST4) acupoint, the needle was inserted towards the direction of the Jiache (ST6) acupoint to a depth of 0.5 to 0.8 inches. Standard needle retention times were maintained for these acupoints.
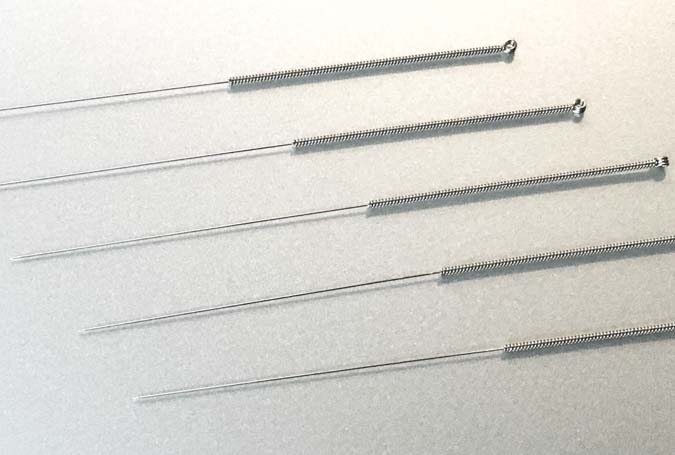
The supplementary acupoints, Baihui and Shangxing, were each treated with 25 mm disposable acupuncture needles. The needles were inserted with a high entry speed, at 15 degrees to the scalp surface. The needles were then manipulated with a high frequency twisting motion with a short-turn rotation technique. Each acupuncture session lasted 30 minutes. Sessions were conducted once daily for 10 consecutive days.
For the massotherapy procedure, rhythmic and gentle rubbing was performed on both the inner and outer sides of the cheeks and around the lips and gums. The root of the tongue received direct pressure and the mandibular area received motion therapy. In addition, the Chengjiang (CV24) and Yongquan (KD1) acupoints received direct acupressure. Each massotherapy session lasted 30 minutes. Sessions were conducted 2 to 3 times daily, for 10 consecutive days. A set of strengthening exercises for the mouth consisted of the following:
- Opening the mouth
- Closing and contracting the mouth
- Rubbing the gums
- Sucking
- Chewing
- Swallowing
One set of exercises was carried out for 10 to 20 minutes at a time, 2 times daily, for 10 consecutive days. For external application on acupoints, the following herbs were applied:
- Gui Zhi (20 g)
- Gan Jiang (20 g)
- Shi Chang Pu (20 g)
- E Zhu (20 g)
- Wu Zhu Yu (20 g)
The ingredients were mixed and ground into powder. The ingredients were combined and 10 g of the mixed herbal powder was combined with vinegar to form an herbal paste. The herbal paste was applied on Yongquan (KD1) bilaterally after skin disinfection. Thereafter, the area was covered with gauze and the gauze was fixed into place with adhesive tape. The herbal paste application was done prior to sleep and removed once the patient woke up in the morning, for 10 consecutive days. The grading system consisted of 5 tiers:
- Grade 1: No drooling
- Grade 2: Slight, occasional drooling
- Grade 3: Ocassional drooling
- Grade 4: Constant, disconnected drooling
- Grade 5: Constant, connected drooling. Chest often wet
The treatment group receiving acupuncture and massotherapy had a shift wherein the majority of patients were Grade 1 (no drooling). The control group had a majority of patients at the Grade 3 level, occasional drooling. Additional objective indices showed cerebral artery blood flow improvements for patient receiving acupuncture and massotherapy. The cerebral artery pulsation index and blood flow peak velocity were more greatly improved in the acupuncture plus massotherapy treatment group than in the control group. Based on the clinical data, acupuncture and massotherapy are safe and effective procedures to help cerebral palsy patients with excessive drooling.
In a related study conducted at the Affiliated Hospital at Nanhua University , Guo et al. conclude that acupuncture benefits hearing for patients with cerebral palsy related hearing impairment. In a surprise finding, acupuncture treatments lasting 30 minutes outperformed longer treatment durations. A total of 90 patients with cerebral palsy related hearing impairment participated in the study. The patients had been diagnosed with the condition between June 2011 to June 2013. They were randomly divided into 3 groups (Group A, Group B, Group C) from the shortest acupuncture treatment duration to the longest respectively.
After treatment, all 3 groups achieved significant reductions in latent and peak periods for wavelength I, III, and V, based on the Brainstem Auditory Evoked Potential (BAEP) evaluation. However, Group A achieved the highest treatment effective rate. The acupoints were the same for all 3 groups:
- Ermen (TB21)
- Tinggong (SI19)
- Tinghui (GB2)
- Yifeng (TB17)
- Jiaosun (TB20)
- Luxi (TB19)
- Chimai (TB18)
Firstly, the patient rested in a supine position and then acupoints were disinfected. A 25 mm acupuncture needle was inserted into each acupoint to a depth of 0.5 to 0.8 inches. The Ping Bu Ping Xie (mild reinforcement and attenuation) manipulation technique was applied for 30 seconds. Subsequently, the following needle retention times were observed for each group:
- Group A: 30 minutes
- Group B: 45 minutes
- Group C: 60 minutes
Each acupuncture session was conducted once daily, for 10 consecutive days, comprising one treatment cycle. The entire course of treatment comprised 3 contiguous treatment cycles. The treatment effective rate was evaluated based on the measurements of the Brainstem Auditory Evoked Potential (BAEP), taken before and after treatment.
The clinical results of the study by Guo et al. demonstrate that acupuncture treatments for cerebral palsy related hearing disorders is effective regardless of acupuncture duration. However, 60 minute and 45 minute treatment durations produced similar treatment results, whereas 30 minute treatment durations produced greater positive patient outcomes. Based on the data, the researchers conclude that 30 minutes is the optimal duration of acupuncture treatments for cerebral palsy related hearing disorders.
The aforementioned studies demonstrate the efficacy of acupuncture for the treatment of cerebral palsy related drooling and hearing impairment. As part of comprehensive treatment regimens, acupuncture demonstrates positive benefits for patients. Based on the findings, additional research is suggested.
References:
Xie AS & Liu LX. (2015). Clinical Observations on Acupuncture and Massotherapy for Cerebral Palsy-salivation. Shanghai Journal of Acupuncture and Moxibustion. 34(6).
Guo, X., Xue, X., Zhou, M., Liu, H. Y. & Li, D. (2015). Clinical Observation of Acupuncture of Different Time Span for Hearing Disorder in Kids with Cerebral Palsy. Shanghai Journal of Acupuncture and Moxibustion. 34 (2).
Wang, P. Q., Zhang, H. J. & Wang, Y. M. (2007). Clinical study on 963 cases of hearing disorder in children with cerebral palsy. China Rehabilitation Theory and Practice. 13 (6): 553-554.
Senner, Jill E., Jerilyn Logemann, Steven Zecker, and Deborah Gaebler‐Spira. "Drooling, saliva production, and swallowing in cerebral palsy." Developmental Medicine & Child Neurology 46, no. 12 (2004): 801-806.


