Acupuncture reduces medication requirements and post-surgical pain for gynecologic laparoscopy patients.
Researchers conclude that acupuncture for gynecologic laparoscopy patients reduces general anesthesia dosage requirements, decreases post-surgical pain, and improves the time to wake and time to fully alert after surgery. In a controlled investigation, acupuncture patients scored better in many other indices as well. Patients having received acupuncture during surgery had increased stability of the heart beat and improved blood pressure upon waking. The results were achieved by applying electroacupuncture to two acupuncture points located on hand and forearm.
Acupuncture improves recovery rates and lowers medication dosages for patients receiving gynecologic laparoscopy, according to research conducted by Huang et al. at the Guangzhou University of Traditional Chinese Medicine. Acupuncture reduced the dosage requirements for general anesthesia. In addition, acupuncture improved time to wake and alertness coming out of general anesthesia. In an important finding, patients receiving acupuncture had significantly less post-surgical pain. Across all of the above indices, patients receiving acupuncture outperformed patients receiving no acupuncture (control group).
The researchers determined that acupuncture successfully alleviates adverse effects associated with general anesthesia. Huang et al. note that the clinical benefits of acupuncture for patients undergoing general anesthesia for gynecologic laparoscopy is attributable to acupuncture’s ability to eliminate pain and regulate blood flow. Acupuncture assists in both lowering dosage requirements for medications while simultaneously providing short and long-term pain relief benefits. The researchers cite Lu whose work entitled Acupuncture combined with medication and anesthesia on abdominal surgery patients and its effects on analgesia published in the Shanghai Journal of Acupuncture indicates that acupuncture combined with general anesthesia stabilizes blood flow mechanics, which speeds up post-surgery recovery.
Anesthesia acupuncture techniques have been used in various types of surgery since the mid-20th century. Huang et al. note that prior clinical research on acupuncture with general anesthesia finds acupuncture effective in minimizing post-surgical physiological damage. Acupuncture relieves pain and regulates the nervous, cardiovascular, digestive, endocrine, and immune systems. As a result, acupuncture reduces adverse effects associated with general anesthesia including dizziness, nausea, regurgitation, flatulence, and urine retention.
Huang et al. used electroacupuncture versus a control group receiving no acupuncture in their clinical trial. The electroacupuncture group required an average of 7.44 mg of propofol and an average of 10.59 ug of remifentanil. The control group required an average of 8.66 mg of propofol and an average of 11.93 ug of remifentanil. These findings are confirmed by additional independent research conducted by Liu et al.
The researchers note that acupuncture’s ability to improve the time to regain consciousness is due to the effects of electroacupuncture allowing for lower doses of medications. The Bispectral Index (BIS) indicates that electroacupuncture allows for greater sedation with lower doses of medications. The electroacupuncture group took 9.05 minutes on average to regain consciousness while the control group took 12.50 minutes on average. The electroacupuncture group took 11.61 minutes on average to regain alertness while the control group took 15.90 minutes on average. The electroacupuncture group significantly outperformed the control group based on the Observer's Assessment of Alertness/Sedation (OAA/S) Scale.
Pain levels were reduced through the implementation of electroacupuncture. The electroacupuncture group reported an average pain score of 3.85 on the Visual Analogue Scale (VAS), shortly after the procedure. The control group experienced greater levels of pain and scored 6.12. Several other measurements indicate that electroacupuncture provides important clinical benefits to patients and doctors. The control group had elevated blood pressure and heart beat levels during awakening. The electroacupuncture group maintained normal blood pressure and heart beat levels at that time. Stable heart beat rates and blood pressure were achieved as a result of electroacupuncture concomitant with general anesthesia.
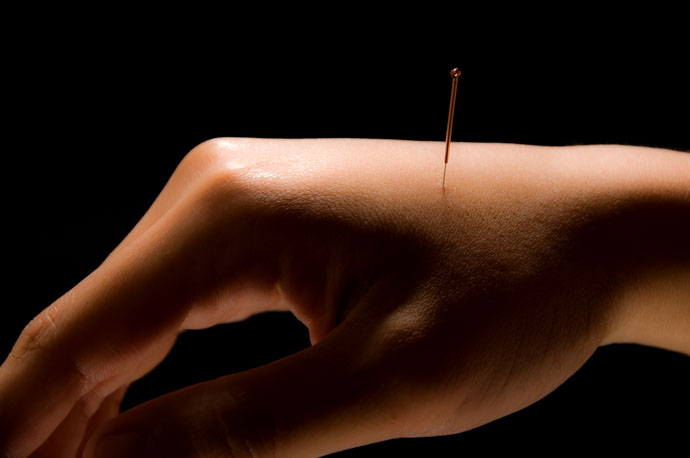
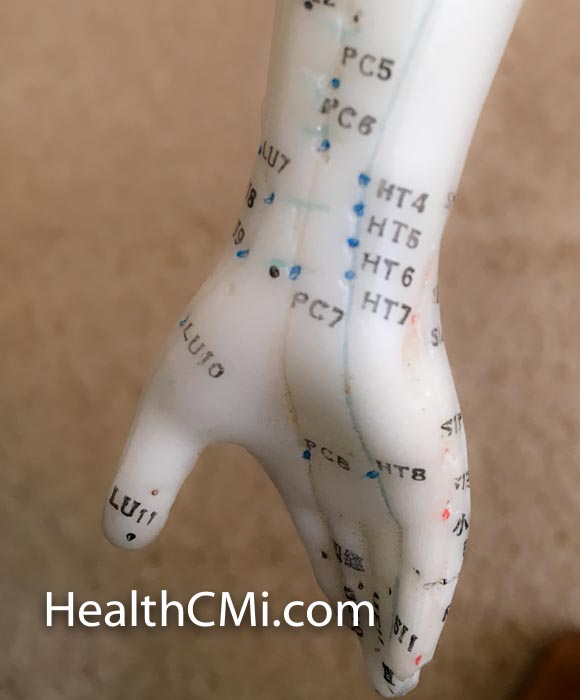
The study involved 60 gynecologic laparoscopy patients. They were randomly divided into two equal groups: electroacupuncture group, control group. The control group received general anesthesia during surgery while the electroacupuncture group received general anesthesia and electroacupuncture during surgery. The acupoints selected for electroacupuncture were applied bilaterally:
- Hegu (LI4)
- Neiguan (PC6)
Electroacupuncture was performed 20 minutes prior to administering general anesthesia and was maintained until the end of the surgery. The procedure started with the patient in a calm state. After standard disinfection on the acupoints, a 30 mm X 25 mm filiform needle was inserted into each acupoint for a depth of 1.5–2 cm. When the patient described the arrival of deqi at the acupoints, the electroacupuncture device was activated with a disperse-dense wave (disperse wave and dense wave, 4 Hz and 20 Hz respectively). The current was limited to 5 mA and adjusted up to this amount, according to individual patient tolerances.
For general anesthesia, plasma target-controlled infusion was used to administer propofol and remifentanil. Propofol is used to slow brain and nervous system activity thereby inducing a state of relaxation. It is a short-acting, lipophilic intravenous general anesthetic that causes global central nervous system depression. Remifentanil is an analgesic opioid that prevents and treats pain by altering pain perception, inhibits pain pathways, and by increasing the pain threshold. The dosages were constantly adjusted during the surgery according to BIS and blood circulation rates. BIS was maintained between 40 and 60 while blood pressure was kept within a 10% margin. Patient consciousness was evaluated based on a modified OAA/S scale, from 0 to 5:
- 5: Responsive to name calling at a normal volume.
- 4: Responsive to name calling at a high volume.
- 3: Responsive to repeated name calling at a high volume, or obtuse response to name calling at a high volume.
- 2: Responsive to slight/medium body shaking.
- 1: Not responsive to body shaking.
- 0: Not responsive to pain stimulation.
Post-surgical pain was evaluated based on the VAS, from 0 to 10 points:
- 0–2 points: No pain.
- 3–4: No obvious pain.
- 5–6: Medium pain.
- 7–8: Heavy pain.
- 9–10: Severe pain.
The clinical results from this study indicate that electroacupuncture greatly improves the quality of post-surgical recovery and health in gynecologic laparoscopy patients, with several indices showing positive outcomes from lowered anesthetic dosages and reduced pain. For this reason, combining acupuncture with general anesthesia provides important health benefits to gynecologic laparoscopy patients.
References:
Huang, Z. P., Xiao, S., Xie, Y. L. & Chen, X. R. (2014). The clinical application of acupuncture combined with general anesthesia in gynecologic laparoscopic surgery. Chinese Journal of Primary Medicine and Pharmacy. 21(20).
Liu, T. Y., Yang, H. Y., Chu, L. X., et al. (2007). Current Research Progress and Analysis of Anesthetic Acupuncture. Journal of China Acupuncture. 27(12):914-915.
Lu, L. (2005). Acupuncture combined with medication and anesthesia on abdominal surgery patient and its effects on analgesia. Journal of Shanghai Acupuncture. 24(4):627.


