Acupuncture is more effective than fluoxetine hydrochloride for the treatment of post-stroke depression. Hebei Medical University Affiliated Cangzhou Hospital of Integrated Traditional Chinese and Western Medicine researchers investigated the effects of acupuncture on patients with post-stroke depression in a randomized controlled clinical trial. For comparison purposes, a control group received fluoxetine hydrochloride. The acupuncture treatment group achieved a total effective rate of 96%; the drug control group achieved an 87% total effective rate.
Acupuncture outperformed fluoxetine hydrochloride (Prozac) across four separate indices (HAMD, NIHSS, Barthel Index, TESS). The HAMD (Hamilton Rating Scale for Depression) measures several important aspects of mental health (e.g., mood, suicidal tendencies, insomnia, interest in work and activities, psychomotor impairment, agitation, anxiety). The NIHSS (NIH Stroke Scale) is a 15 item neurologic examination of stroke adverse effects. The Barthel Index (BI) measures the ability to live independently based on mobility and activities of daily living performance (e.g., eating, bathing, dressing, walking, bladder and bowel control). TESS (Treatment Emergent Symptom Scale) measures the safety and efficacy of treatment. At the 96% total effective rate, the acupuncture group outperformed the drug control group across all tested indices by 9%.
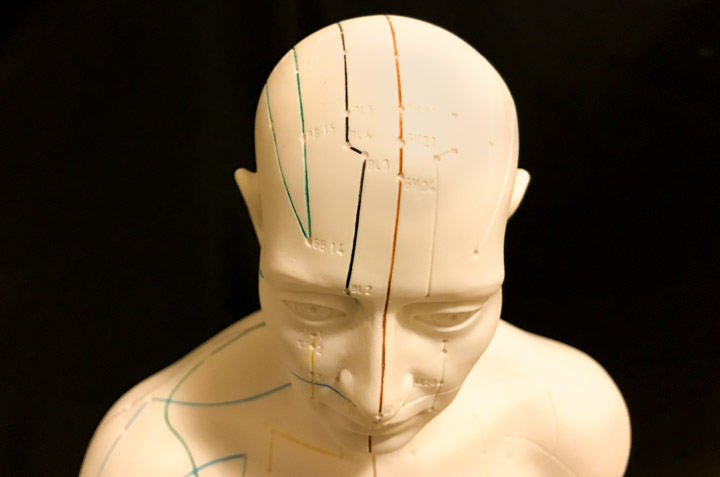
Darer et al. note that at the one year data point after a stroke, the incidence rate of post-stroke depression is 20% to 30%, which peaks within 6 months after a stroke. Stroke patients often experience severe psychological challenges. Many of the psychological disturbances result from stroke related disabilities (e.g., motor dysfunction, dysphagia, speech disorders, urinary and fecal difficulties). If patients do not receive timely treatment and remain depressed for a prolonged period of time, it negatively affects the recovery process. The researchers tested the efficacy of the Xing Nao An Shen Tong Luo (mind revitalization, tranquilizing, and meridian dredging) acupuncture technique. Primary acupoints treated include:
- Baihui (DU20)
- Sishencong (Extra)
- Shenting (DU24)
In addition, twelve Jing-Well acupoints were needled. Baihui is a Governing meridian acupoint located on the vertex. Traditional Chinese Medicine (TCM) principles indicate the use of the chosen acupuncture point prescription. The researchers sought to test the TCM approach to care with modern testing methods.
According to TCM principles, acupuncture at Baihui dredges the Governing meridian and revitalizes the mind. Sishencong is a series of four acupoints surrounding the vertex. Acupuncture at Sishencong is indicated for benefitting the brain and intellect. Sishencong is also indicated for inducing tranquility. Shenting is used for its shen calming properties and also for its ability to benefit the brain. The application of the twelve Jing-Well acupoints (Da Jie Jing Fa) promotes blood circulation, dredges the meridians, and calms the spirit.
The Xing Nao An Shen Tong Luo (mind refreshing, tranquilizing, and meridian dredging) needling technique emphasizes manual acupuncture stimulation, needling direction, and elicitation of a deqi sensation. Primary acupoints treated include Baihui, Sishencong, Shenting, and the twelve Jing-Well acupoints. All needles were 0.30 mm x 40 mm Hao acupuncture needles. The Baihui acupoint was needled posteriorly at a transverse-oblique angle to a depth of 0.8 – 1 inches. Sishencong was needled transverse-obliquely towards the direction of the Baihui acupoint to a depth of 0.5 – 0.8 inches. Shenting was needled transverse-obliquely toward the direction of the Baihui acupoint to a depth of 0.8 – 1 inches to the level above the galea aponeurotica.
Acupuncture needles were evenly rotated at a rate of 120 rotations per minute. The intensity of needle manipulation was adjusted to induce a sensation of deqi soreness. The duration of needle manipulation was one minute per acupuncture session. Treatments were applied once per day for a total of 8 weeks. The needle retention time was 30 minutes per acupuncture session, during which the acupuncture needles were manipulated once.
In addition to filiform needle acupuncture treatments, the treatment group also received Ci Luo (meridian pricking) treatments. Twelve Jing-Well acupoints were treated in the following order: Shaoshang, Shangyang, Lidui, Yinbai, Shaochong, Shaoze, Zhiyin, Yongquan, Zhongchong, Guanchong, Zuqiaoyin, Dadun. The skin was disinfected prior to needling. Next, a three edged needle was applied to the acupoints on the side affected by the stroke. Next, the acupoints on the healthy side were needled. On each finger, 1 – 3 drops of blood were squeezed from the Jing-Well acupoints. This treatment was applied once every other day, for a total of 8 weeks. The drug control group received fluoxetine hydrochloride capsules (20 mg/day) daily for 8 weeks.
The results of the investigation demonstrates that acupuncture is safe and effective for the relief of post-stroke depression. In related research, Guangdong Chinese Medicine School researchers find acupuncture beneficial for post-stroke patients. Patients receiving acupuncture had a 90% total effective rate for the recovery of motor abilities. In addition, 46.67% of patients achieved very significant motor improvements. Brunnstrom Approach upper and lower limb motor abilities significantly improved and the Barthel Activities of Daily Living (ADL) index improving from a 38.80 to a 55.80. Acupuncture points used in the study included the following:
- Neiguan (PC6)
- Sanyinjiao (SP6)
- Jiquan (HT1)
- Chize (LU5)
- Weizhong (BL40)
- Renzhong (DU26)
Abdominal acupuncture points were applied on alternating days and supplementary acupoints were added for specific disorders. For aphasia, Jinjin and Yuye were added. For dysphagia, Yifeng (SJ17) and Fengchi (GB20) were added. For deviation of the mouth, Jiache (ST6) was added. Quchi (LI11) and Waiguan (SJ5) were added for pain and impaired movement of the upper limbs. For finger spasticity, Hegu (LI4) and Houxi (SI3) were added. Bafeng and Baxie were added for sensory disorders of the feet and hands.
Guangzhou University of Chinese Medicine researchers (Yang et al.) investigated the biological effects of acupuncture on the brain. Their investigation finds acupuncture effective in the stimulation of angiogenesis and nerve repair after cerebral ischemia. Acupuncture at GV20 (Baihui) and GV14 (Dazhui) increases the expression of VEGF (vascular endothelial growth factor) and Ang-1 (angioprotein 1) in the area of a cerebral ischemic focus. In addition, acupuncture at these acupoints affects the expressions of signal transducers and activators of transcription (STATs). The researchers note that regulation of STATs indicates that acupuncture activates self-protection and reduction of “apoptosis of the nerve cells in and around the ischemic focus.”
Yang et al. note that acupuncture on the CV and GV channels promotes “proliferation and differentiation of NSCs in the ischemic brain.” NSCs (neural stem cells) in the brain maintain the “ability of self-duplication, self regeneration and continuous differentiation into neuron and neuroglial cells.” The researchers add, needling acupoints GV20 (Baihui) and GV26 (Shuigou) “increase(s) the release of nerve growth factors (NGFs) to make nerve cells survive and axons grow, synthesize neurotransmitters, [and] metabolize toxic substances. . . .” Moreover, needling CV24 (Chengjiang), CV4 (Guanyuan), GV26 (Shuigou), and GV20 (Baihui) “inhibit(s) excessive proliferation of the hippocampal astrocytes and promote cellular differentiation.” In summation, acupuncture demonstrates the ability to benefit post-stroke patients in both subjective and objective data.
References
Song SC, Lu Z, Wang RY & Chen H. (2014). Interventive Effect of Acupuncture in the Treatment of Post-stroke Depression and Neurological Functional Rehabilitation. JCAM. 30(10).
Zhang, G. F., Huang, Y. & Zeng, T. J. (2014). Therapeutic Effect of Activating Brain and Regaining Consciousness Needling Combined with Bo’s Abdomen Acupuncture on Stroke Sequelae: Analysis of 30 Cases. Journal of Clinical Acupuncture and Moxibustion. 30 (4).
Feng, F. Z. (2013). Activating Brain and Regaining Consciousness (Xing Nao Kai Qiao) Needling Technique for the Early Treatment of Acute Phase Stroke: 120 Cases. Chinese Medicine Modern Distance Education of China. 17 (4): 59-61.
Darer RM, Rao M, Shareef A, et al. Post stroke depression. Top Stroke Rehabil, 2008, 15(1): 13-21.
Zhou-xin Yang, Peng-dian Chen, Hai-bo Yu, Wen-shu Luo, Yong-Gang Wu, Min Pi, Jun-hua Peng, Yong-feng Liu, Shao-yun Zhang, Yan-hua Gou. Research advances in treatment of cerebral ischemic injury by acupuncture of conception and governor vessels to promote nerve regeneration. Journal of Chinese Integrative Medicine, Jan. 2012. vol. 10, 1. Department of Acupuncture and Moxibustion, Shenzhen Traditional Chinese Medicine Hospital, Guangzhou University of Chinese Medicine, Guangdong Province, China.


