At the Healthcare Medicine Institute, we have received the most acupuncture information requests about the following research publications in the last several months. Below are excerpts from the articles that feature important acupuncture research and clinical findings. Enjoy the top 7 acupuncture aricles of the spring and summer on the following topics:
- Acupuncture For Fertility
- Acupuncture and the American College of Physicians
- Nerve Repair and Acupuncture
- Antiinflammatory Acupuncture
- Acupuncture Reduces Pain Levels
- MRI and Acupuncture
- Biochemical Changes and Acupuncture
Acupuncture For Fertility
In our first article of the top 7, researchers find acupuncture combined with clomiphene more effective than clomiphene plus supplementary hormonal pharmaceuticals for the treatment of infertility. The combination of acupuncture plus clomiphene produces significantly higher pregnancy rates for women with anovulatory infertility than clomiphene plus estradiol cypionate and dydrogesterone. The data was published in the report entitled Effects of Acupuncture on the Endometrium in Anovulatory Cases Treated by Clomiphene: A Clinical Observation.
The addition of acupuncture to clomiphene therapy increased pregnancy rates, lowered the resistance and pulsatility indices of the uterine arteries, and reduced the adverse effects caused by clomiphene. The increase in positive patient outcomes combined with reductions of adverse effects supports the research team’s (Taian Maternal and Child Health Care Hospital) conclusion, “TCM [Traditional Chinese Medicine] can be either applied alone or combined with Western medicine to up pregnancy rates and treat infertility. With the help of TCM [i.e., acupuncture], treatment for infertility can be more effective while producinag much less adverse effects.”
The researchers conclude that the addition of acupuncture to a clomiphene treatment regimen mitigates the drug’s adverse effects and ups the pregnancy rate. Moreover, the acupuncture protocol outperforms the clomiphene plus estradiol cypionate and dydrogesterone protocol.
The TCM acupuncture treatment protocol was as follows. Patients rested in a supine position. Upon disinfection, a 0.30 mm x 40 mm filiform needle was inserted into the following acupoints:
- CV4 (Guanyuan)
- CV3 (Zhongji)
- Zigong
- ST29 (Guilai)
- SP6 (Sanyinjiao)
- ST36 (Zusanli)
CV4, CV3, Zigong, and ST29 were inserted transverse-obliquely (15° angle) to a depth of 1–1.2 cm. SP6 and ST36 were needled perpendicularly and manipulated with the Ping Bu Ping Xie (tonify and sedate) technique. Additional acupoints were administered based on differential diagnostic patterns. For liver qi stagnation, the following acupoint was added:
- BL18 (Ganshu)
For phlegm and dampness, the following acupoint was added:
- ST40 (Fenglong)
For blood stasis, the following acupoints were added:
- SP10 (Xuehai)
- LV2 (Xingjian)
Moxibustion sessions lasted 30 minutes and were applied at a heat intensity level until the skin became flushed. Sessions were conducted once per day. Moxibustion was not applied until 10 days passed after ovulation. Moxibustion was applied at the following acupoints:
- Zigong
- CV3 (Zhongji)
- CV4 (Guanyuan)
- ST29 (Guilai)
References
Effects of Acupuncture on the Endometrium in Anovulatory Cases Treated by Clomiphene: A Clinical Observation. Journal of Taishan Medical College. 2016, 37(9):1029-1031.
Yu J, Zheng HM, Bing SM. Changes in sSrum FSH, LH and Ovarian Follicular Growth During Electroacupuncture for Induction of Ovulation [J]. Chinese Journal of Integrated Traditional and Western Medicine. 1989, 9(4):199-202.
Sha GE, Huang WC, Ma RH. Acupuncture for Infertility: A Clinical Observation Based on 84 cases [J]. Journal of Clinical Acupuncture and Moxibustion. 1998, 14(1):16-18.
Xu XF, Gu Y, Gu Ling, Zhu YP. Investigating Advantages of TCM Intervention for Inducting Ovulation in Infertile Women [J]. Chinese Archives of Traditional Chinese Medicine. 2012, 30(3):467-468.
Cao ZY. Obstetrics and Gynecology [M]. Beijing: People's Military Medical Publisher. 1999: 2474.
Manheimer, Eric, Daniëlle van der Windt, Ke Cheng, Kristen Stafford, Jianping Liu, Jayne Tierney, Lixing Lao, Brian M. Berman, Patricia Langenberg, and Lex M. Bouter. "The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: a systematic review and meta-analysis." Human reproduction update (2013). University of Maryland.
Acupuncture and the American College of Physicians
The American College of Physicians formally recommends acupuncture for the treatment of back pain. Published in the prestigious Annals of Internal Medicine, clinical guidelines were developed by the American College of Physicians (ACP) to present recommendations based on evidence. Citing quality evidence in modern research, the ACP notes that nonpharmacologic treatment with acupuncture for the treatment of chronic low back pain is recommended. The official grade by the ACP is a “strong recommendation.”
A strong recommendation is also made by the American College of Physicians for the treatment of both acute and subacute lower back pain with heat, massage, acupuncture, and spinal manipulation. The recommendations were approved by the ACP Board of Regents and involves evidence based recommendations from doctors at the Penn Health System (Philadelphia, Pennsylvania), Minneapolis Veterans Affairs Medical Center (Minnesota), and the Yale School of Medicine (New Haven, Connecticut). The target audience for the American College of Physicians recommendations includes all doctors, other clinicians, and the adult population with lower back pain. The ACP notes, “Moderate-quality evidence showed that acupuncture was associated with moderately lower pain intensity and improved function compared with no acupuncture at the end of treatment .” In agreement, the National Institute of Neurological Disorders and Stroke (National Institutes of Health) notes that acupuncture is an effective treatment modality for the relief of chronic lower back pain.
References
1. Qaseem, Amir, Timothy J. Wilt, Robert M. McLean, and Mary Ann Forciea. "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of PhysiciansNoninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain." Annals of Internal Medicine (2017).
2. Qaseem, et al. Annals of Internal Medicine (2017).
3. Katz J.N. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences.J Bone Joint Surg Am200688 Suppl 2214.
4. Lam M. Galvin R. Curry P. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta-analysis.Spine (Philadelphia, Pennsylvania 1976) 201338212438.
5. ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet. Low Back Pain Fact Sheet, National Institute of Neurological Disorders and Stroke, National Institutes of Health.
6. Nahin, Richard L., Robin Boineau, Partap S. Khalsa, Barbara J. Stussman, and Wendy J. Weber. "Evidence-based evaluation of complementary health approaches for pain management in the United States." In Mayo Clinic Proceedings, vol. 91, no. 9, pp. 1292-1306. Elsevier, 2016.
7. Martin DP, Sletten CD, Williams BA, Berger IH. Improvement
in fibromyalgia symptoms with acupuncture: results of a randomized
controlled trial. Mayo Clin Proc. 2006;81(6):749-757.
8. MacPherson, H., A. Vickers, M. Bland, D. Torgerson, M. Corbett, E. Spackman, P. Saramago et al. "Acupuncture for chronic pain and depression in primary care: a programme of research." (2017).
9. Leslie Lingaas. ucsf.edu/news/2014/04/113966/acupuncture-helps-young-patients-manage-pain. Acupuncture Helps Pediatric Patients Manage Pain and Nausea, 2014.
10. Lin, Lili, Nikola Skakavac, Xiaoyang Lin, Dong Lin, Mia C. Borlongan, Cesar V. Borlongan, and Chuanhai Cao. "Acupuncture-induced analgesia: the role of microglial inhibition." Cell transplantation 25, no. 4 (2016): 621-628.
11. Cevic, C and Iseri, SO. The effect of acupuncture on high blood pressure of patients using antihypertensive drugs. Acupuncture & electro-therapeutics research 2013; 38(1-2).
Nerve Repair and Acupuncture
Acupuncture repairs injured nerves. Findings published in Neural Regeneration Research demonstrate that acupuncture causes injured lower and upper limb motor nerves to repair. Electromyographic nerve conduction tests of acupuncture patients with nerve injuries document “an effective response” in 80% of patients participating in the study.
Electromyography confirms that acupuncture significantly improves motor nerve conduction velocity and amplitude and also promotes functional nerve repair. The researchers made an important discovery. A special set of acupuncture points resulted in good to excellent clinical responses at a very high rate. Using only local acupuncture points, patients had an effective rate of 38.5%. By adding acupuncture points to the Du meridian in addition to local acupuncture points, the effective rate jumped to 80%.
The Du meridian is a pathway composed of 28 primary acupuncture points plus extra acupoints. Many of the Du meridian acupuncture points are located on the midline of the back below the spinous processes of the vertebrae. In Traditional Chinese Medicine (TCM), the application of acupuncture points to the Du meridian (Governor vessel) are used for the treatment of many disorders including spine and brain ailments, vertigo, numbness, tremors, febrile diseases, and infertility.
The research published in Neural Regeneration Research confirms the Du meridian’s significant role in the treatment of nerve injuries. Electroacupuncture was applied to both the upper and lower limb groups at a rate of once per day, five times per week for a total of six weeks. The total number of acupuncture treatments was 30 sessions per patient. The researchers conclude, “Our results indicate that Governor vessel and local meridian acupoints used simultaneously promote functional repair after peripheral nerve injury.”
The acupuncture points used in the study were a protocolized set of two acupuncture point prescriptions, one for the upper limbs and one for the lower limbs. The upper limb acupuncture point prescription consisted of local acupoints at the site of the injured nerve plus the following Du meridian acupoints:
- Baihui (DU20)
- Fengfu (DU16)
- Dazhui (DU14)
- Shenzhu (DU12)
The lower limb acupuncture point prescription consisted of local meridian acupoints at the site of the injured nerve plus the following Du meridian acupoints:
- Jizhong (DU6)
- Mingmen (DU4)
- Yaoyangguan (DU3)
- Yaoshu (DU2)
The local acupuncture points used in the study were chosen based on the area of nerve injury. Radial nerve injuries were treated with the following acupuncture points:
- Jianyu (LI15)
- Binao (LI14)
- Quchi (LI11)
- Hegu (LI4)
- Yangxi (LI5)
Ulnar nerve injuries were treated with the following acupuncture points:
- Qingling (HT2)
- Xiaohai (SI8)
- Zhizheng (SI7)
- Wangu (SI4)
- Houxi (SI3)
Median nerve injuries were treated with the following acupuncture points:
- Quze (PC3)
- Daling (PC7)
- Neiguan (PC6)
- Laogong (PC8)
Peroneal nerve injuries were treated with the following acupuncture points:
- Yanglingquan (GB34)
- Guangming (GB37)
- Juegu (GB39)
- Qiuxu (GB40)
Tibial nerve injuries were treated with the following acupuncture points:
- Yinlingquan (SP9)
- Sanyinjiao (SP6)
- Diji (SP8)
- Lougu (SP7)
Sciatic nerve injuries were treated with the following acupuncture points:
- Huantiao (GB30)
- Ciliao (BL32)
- Zhibian (BL54)
- Yanglingquan (GB34)
- Weizhong (BL40)
- Juegu (GB39)
Brachial plexus injuries were treated with the following acupuncture points:
- Jianyu (LI15)
- Binao (LI14)
- Quchi (LI11)
- Waiguan (SJ5)
- Baxie (EX-UE8)
The acupuncture needles were 0.35 x 25 mm and were applied to an approximate depth of 1 cun at each acupoint. Manual acupuncture was applied to elicit a response followed by application of electroacupuncture with a sparse-dense wave between 2 - 100 Hz. Intensity was set to tolerance levels.
The researchers note that nerve injuries affect the metabolic microenvironment. Citing an example, they note that sciatic nerve injuries reduce acetylcholinesterase activity in the lumbar spinal cord microenvironment. This causes neuronal cell death thereby impeding nerve repair. The researchers note that acupuncture counteracts this effect citing that it successfully increases “acetylcholinesterase expression in spinal cord tissue after peripheral nerve injury.” As a result, the researchers suggest that this may be an important mechanism by which acupuncture promotes the healing of peripheral nerves.
Reference
Gh, He, Ruan Jw, Zeng Ys, X. Zhou, Y. Ding, and Zhou Gh. "Improvement in acupoint selection for acupuncture of nerves surrounding the injury site: electro-acupuncture with Governor vessel with local meridian acupoints." Neural Regeneration Research 10, no. 1 (2015): 128.
Antiinflammatory Acupuncture
Acupuncture reduces inflammation and researchers have discovered how it works. In a laboratory controlled scientific investigation, a key biological marker has been identified, quantified, and directly correlated with the application of acupuncture. Acupuncture successfully downregulates a proinflammatory biochemical (tumor necrosis factor alpha), which results in anti-inflammatory responses. In addition, the researchers have mapped the neural pathways by which acupuncture signaling stimulates anti-inflammatory effects.
Researchers in Korea have identified a mechanism by which acupuncture stimulation at the acupoint ST36 (Zusanli) has an anti-inflammatory effect. By downregulating tumor necrosis factor alpha (TNF-α), acupuncture relieves systemic inflammation. By testing the effects that a splenic neurectomy and vagotomy have on TNF-α levels in the spleen and the brain, Lim et al. found that the anti-inflammatory effects of ST36 (Zusanli) rely on the vagus nerve pathway. Both manual acupuncture stimulation (MAC) and electroacupuncture (EAC) induce c-Fos protein generation. However, only manual acupuncture stimulation has the effect of downregulating TNF-α; electroacupuncture has the opposite effect when applied to ST36.
Chronic inflammation is involved in a variety of disease processes. Inflammation is part of the body’s natural response to injuries, but if the condition persists it can lead to further damage. There are a number of factors related to chronic inflammation, including TNF-α. As an endogenous pyrogen, TNF-α is primarily involved in the regulation of immune cells. It is able to induce fever, inflammation, apoptosis, inhibit tumor growth, and inhibit virus replication. However, its dysregulation is implicated in the processes of a number of diseases including major depression, cancer, psoriasis, Alzheimer’s disease, and inflammatory bowel disease (IBD). The researchers in this study used lipopolysaccharide (LPS) to induce TNF-α production in lab mice. Next, they performed a real-time polymerase chain reaction (PCR) DNA analysis, which “showed that TNF-α mRNA was highly induced in the spleen following LPS administration and was downregulated by MAC.”
The researchers also gave the mice either a splenic neurectomy or a vagotomy to discern which nerve pathway was responsible for transmitting the anti-inflammatory responses induced by the acupuncture treatments. They found that the TNF-α levels decreased with MAC but were re-elevated in mice with a splenic neurectomy and vagotomy, suggesting that “TNF-α induced in the spleen and the serum after LPS administration may be modulated by AS [acupuncture stimulation].” Another trial showed that CNQX (AMPA receptor blocker) and PPADS (selective purinergic antagonist) — which both inhibit the dorsal vagal complex (DVC) — also decreased splenic TNF-α, which implies the direct involvement of the vagus nerve in the modulation of TNF-α.
The vagus nerve is a cranial nerve best known for innervating the viscera. However, “growing bodies of evidence indicate that vagus nerve activity is important not only for homeostatic regulation of internal organs but also for the regulation of pathologic inflammatory reactions; thus, the vagus nerve acts as a bridge between the neural and immune systems. Notably, VNS can activate the a7 nicotinic acetylcholine receptor on the macrophages in the spleen.”
The cholinergic response, mediated by the vagus nerve, directly controls a proinflammatory response by way of the inflammatory reflex. Several inflammatory diseases are regulated by the ‘cholinergic anti-inflammatory reflex,’ including rheumatoid arthritis, diabetes, and obesity. Additionally, previous research finds that insulin resistance is caused by chronic inflammation resulting from immune and metabolic dysregulation; in addition, a decrease in vagus nerve activity is correlated with obesity. “Selective cholinergic activation within the efferent vagus nerve-mediated arm of the inflammatory reflex can suppress obesity-associated inflammation and reverse metabolic complications. These findings raise the intriguing possibility that dysregulation of vagus nerve-mediated signaling might contribute to the pathogenesis of obesity and its related comorbidities.”
Obesity has reached epidemic levels in many countries and is a precursor for many chronic diseases, including diabetes. Chronic inflammation is “a critical step in the pathogenesis of insulin resistance and type 2 diabetes mellitus. Cholinergic mechanisms within the inflammatory reflex have, in the past 2 years, been implicated in attenuating obesity-related inflammation and metabolic complications. This knowledge has led to the exploration of novel therapeutic approaches in the treatment of obesity-related disorders.”
References
HD Lim et al., “Anti-Inflammatory Effects of Acupuncture Stimulation via the Vagus Nerve,” PloS one. 11, no. 3 (March 19, 2016), accessed February 3, 2017, pp 4-5. ncbi.nlm.nih.gov/pubmed/26991319
Valentin A. Pavlov and Kevin J. Tracey, The Vagus Nerve and the Inflammatory Reflex—linking Immunity and Metabolism, 8, no. 12, accessed February 3, 2017, ncbi.nlm.nih.gov/pmc/articles/PMC4082307/
Yun-Kyoung Yim et al., Electro-Acupuncture at Acupoint ST36 Reduces Inflammation and Regulates Immune Activity in Collagen-Induced Arthritic Mice, 4, no. 1 (August 18, 2006), accessed February 3, 2017, ncbi.nlm.nih.gov/pmc/articles/PMC1810363/
Lin, Lili, Nikola Skakavac, Xiaoyang Lin, Dong Lin, Mia C. Borlongan, Cesar V. Borlongan, and Chuanhai Cao. "Acupuncture-induced analgesia: the role of microglial inhibition." Cell transplantation 25, no. 4 (2016): 621-628.
Zhang, Ruixin, Lixing Lao, Ke Ren, and Brian M. Berman. "Mechanisms of acupuncture–electroacupuncture on persistent pain." The Journal of the American Society of Anesthesiologists 120, no. 2 (2014): 482-503.
Acupuncture Reduces Pain Levels
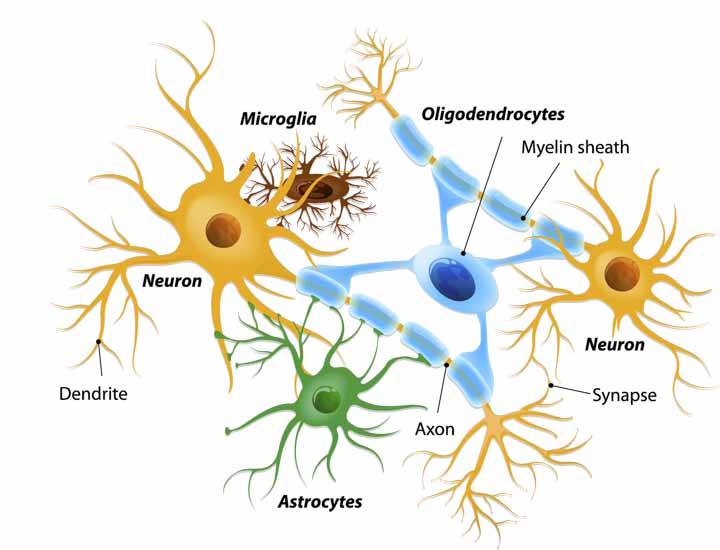
Acupuncture is effective for pain relief. Researchers from the University of South Florida (Tampa) and the Fujian University of Traditional Chinese Medicine (Fuzhou) document that acupuncture alleviates pain, in part, by regulation of microglial cells. These are non-neural cells that comprise part of the central nervous system structure. Scientists already knew that microglial cells act as macrophages at sites of damaged central nervous system tissue. The research team (Lin et al.) from the University of South Florida (Department of Neurosurgery and Brain Repair, Department of Pharmaceutical Sciences) along with researchers from the Fujian University of Traditional Chinese Medicine (College of Acupuncture) made the key findings.
The researchers cite evidence demonstrating that acupuncture inhibits “microglial and astrocytic proliferation coupled with improved functional recovery after SCI [spinal cord injury].” They add, “acupuncture exerts a remarkable analgesic effect on SCI by also inhibiting production of microglial cells through attenuation of p38MAPK and ERK activation.” The researchers note that their investigation summarizes “clinical evidence demonstrating that acupuncture is capable of producing analgesia in neuropathic pain by suppressing microglial activation.” Funding for the groundbreaking research was provided by the US Department of Defense, University of South Florida Neurosurgery and Brain Repair, and the James and Esther King Biomedical Research Foundation.
The researchers note that scientists find both microglia and astrocytes involved in inflammation and pain. In addition, the researchers cite evidence demonstrating that acupuncture has an inhibitory effect on microglial activation. The research team provides background to this information. Microglia are the primary immune system cells in the central nervous system. They secrete proinflammatory and neurotoxic mediators when activated. The release of these mediators creates a positive feedback loop that leads to increased reactive oxygen species (ROS) induced microglial activation and subsequent inflammatory responses. Since acupuncture inhibits ROS, the researchers note that their findings “provide the possibility that acupuncture can be used effectively as a nonpharmacological intervention for spinal cord injury (SCI)-induced chronic neuropathic pain in patients.” They add that acupuncture has an important benefit to the brain. Electroacupuncture alleviates oxidative damage to the hippocampus by “preventing microglial activation.”
Lin et al. cited specific acupuncture points shown to elicit specific microglial responses. Electroacupuncture at GB20 (Huantiao) and GB34 (Yanglingquan) “significantly suppressed CFA-induced nociceptive behavioral hypersensitivity and spinal microglial activation.” Freund's Complete Adjuvant (CFA) is comprised of inactive mycobacteria, often used for stimulating cell mediated immunity responses in research. Moreover, when electroacupuncture was combined with a microglial inhibitor drug, the pain relieving effects of electroacupuncture were enhanced for cases of allodynia and hyperalgesia. The research team adds several other examples of microglial attenuation by acupuncture, including the ability of manual acupuncture to downregulate MAC-1 (macrophage-1 antigen), an indicator of microglial activation.
Lin et al. discussed other mechanisms shown to alleviate pain by modern research. They note that acupuncture stimulates the release of neurotransmitters, including opioids, in the central nervous system (2,3,4). The researchers add that this causes “potent analgesia, regulation of visceral functions, and immune modulation.” Lin et al. add that electroacupuncture enhances natural killer (NK) cell activity and beta-endorphin production via the hypothalamus.
The research team notes that numerous MRI (magnetic resonance imaging) studies find electroacupuncture effective for the activation of the hypothalamus. In one study cited by the team, researchers find “evidence suggesting that chronic pain patients respond to acupuncture differently than HC [healthy controls], through a coordinated limbic network including the hypothalamus and amygdala (Napadow et al.).”
Napadow et al. used fMRI data to compare true acupuncture with sham acupuncture for patients with carpal tunnel syndrome. The acupuncture point LI4 (Hegu) was tested. Both short-term and long-term responses were measured. True acupuncture at the real acupuncture point stimulated significantly “greater activation in the hypothalamus and deactivation in the amygdala” for patients with carpal tunnel syndrome. The research team was comprised of Massachusetts General Hospital (Charlestown), Spaulding Rehabilitation Hospital (Boston, Massachusetts), and Logan College of Chiropractic (Chesterfield, Missouri) researchers.
Lin et al. note that numerous studies find acupuncture effective for the relief of pain; however, the mechanisms of action were unknown. For example, University of Manchester (UK) researchers (Abuaisha et al.) note, “acupuncture is a safe and effective therapy for the long-term management of painful diabetic neuropathy, although its mechanism of action remains speculative.” Lin et al. add that researchers at the Toronto Rehabilitation Institute in the Lyndhurst Centre (Toronto, Ontario, Canada) also found acupuncture clinically effective but did not map the mechanisms of effective action. The Toronto Rehabilitation Institute researchers concluded, “This retrospective study suggests that the Lyndhurst Center Central Neuropathic Pain Acupuncture Protocol may be an effective treatment option for patients with SCI who are experiencing below-level central neuropathic pain.”
Lin et al. provided another important example of clinical results with a call for greater inquiry into the mechanisms of effective action. Researchers from the University of Maryland (Baltimore) conclude, “Electroacupuncture blocks pain by activating a variety of bioactive chemicals through peripheral, spinal, and supraspinal mechanisms. These include opioids, which desensitize peripheral nociceptors and reduce proinflammatory cytokines peripherally and in the spinal cord, and serotonin and norepinephrine, which decrease spinal N-methyl-d-aspartate receptor subunit GluN1 phosphorylation.” Given the results of their research, the University of Maryland team (Zhang et al.) adds, “Clarification of acupuncture/electroacupuncture mechanisms will open a variety of opportunities to combine acupuncture/electroacupuncture with medications to manage and control pain, which makes it all the more important to continue such research.” The University of Maryland study was published in the The Journal of the American Society of Anesthesiologists.
Lin et al. note that mechanisms of action have been explored in a variety of research. For example, Xiao et al. conclude that “P2X3 receptors in the lPAG [lateral midbrain periaqueductal gray] are involved in the supraspinal antinociception effect of EA [electroacupuncture] treatment.” Lin et al. note that the details of the research by Xiao et al. reveal that PAG (midbrain periaqueductal gray) is an important brain structure active in electroacupuncture pain regulation.
Lin et al. made significant findings. They note that acupuncture modulates homeostasis and alleviates pain. In addition, acupuncture activates areas of the central nervous system including the PAG and nucleus raphe magnus. In addition, acupuncture deactivates areas of the limbic system thereby regulating emotions correlated with pain.
References
1. Lin, Lili, Nikola Skakavac, Xiaoyang Lin, Dong Lin, Mia C. Borlongan, Cesar V. Borlongan, and Chuanhai Cao. "Acupuncture-induced analgesia: the role of microglial inhibition." Cell transplantation 25, no. 4 (2016): 621-628.
2. Han, J. S. Acupuncture neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 26(1):17–22; 2003.
3. Mori, H.; Nishijo, K.; Kawamura, H.; Abo, T. Unique immunomodulation by electro-acupuncture in humans possibly via stimulation of the autonomic nervous system. Neurosci. Lett. 320(1–2):21–24; 2002.
4. Sato, A.; Schmidt, R. F. The modulation of visceral functions by somatic afferent activity. Jpn. J. Physiol. 37(1):1–17; 1987.
5. Napadow, V., N. Kettner, J. Liu, M. Li, K. K. Kwong, M. Vangel, N. Makris, J. Audette, and K. K. S. Hui. "Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome." Pain 130, no. 3 (2007): 254-266.
6. Abuaisha, B. B., J. B. Costanzi, and A. J. M. Boulton. "Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: a long-term study." Diabetes research and clinical practice 39, no. 2 (1998): 115-121.
7. Zhang, Ruixin, Lixing Lao, Ke Ren, and Brian M. Berman. "Mechanisms of acupuncture–electroacupuncture on persistent pain." The Journal of the American Society of Anesthesiologists 120, no. 2 (2014): 482-503.
8. Xiao, Zhi, Shan Ou, Wen-Juan He, Yan-Dong Zhao, Xiao-Hong Liu, and Huai-Zhen Ruan. "Role of midbrain periaqueductal gray P2X3 receptors in electroacupuncture-mediated endogenous pain modulatory systems." Brain research 1330 (2010): 31-44.
MRI and Acupuncture
MRI studies reveal the neurological mechanisms of acupuncture on human health. Research published in Autonomic Neuroscience demonstrates that stimulation of specific acupuncture points induces hemodynamic changes in specific brain networks. The researchers add that brain networks accessed by specific acupuncture points relate to specific medical disorders and suggest an “acupoint-brain-organ” pathway.
Functional magnetic resonance imaging (fMRI) studies reveal specific acupuncture point effects in the brain through blood-oxygen-level dependent (BOLD) measurements. In a meta-analysis of 82 fMRI studies, researchers found a large body of evidence supporting acupuncture point specificity. This applies to both manual acupuncture and electroacupuncture. True acupuncture point stimulation induced specific cortical effects whereas sham acupuncture did not. In addition, the researchers note that acupuncture point stimulation produces significantly “more positive and negative hemodynamic signal response(s) in brain regions compared with sensory stimulation used as a control condition.”
Many important findings were confirmed. Acupuncture exerted a stimulus that “could induce beneficial cortical plasticity in carpal tunnel syndrome patients.” It was also demonstrated that acupuncture relieved pain “by regulating the equilibrium of distributed pain-related central networks.”
The researchers note that a fundamental principle of Traditional Chinese Medicine (TCM) is that “specific acupoints have therapeutic effects on target organ systems remote from the needling site….” Recent fMRI investigations support this principle. The researchers note that “fMRI investigations regarding several acupoints have demonstrated that acupuncture stimulation at disorder-implicated acupoints modulates the activity of the disorder-related brain regions.”
In TCM, acupuncture point Neiguan (PC6) is indicated for the treatment of nausea and vomiting. The fMRI research supports this ancient principle. The researchers note, “Acupuncturing at Neiguan (PC6) could selectively evoke hemodynamic response of insula and cerebellar-hypothalamus in order to exert modulatory effects on vestibular functions, indicating the specific treatment effect on nausea and vomiting.”
Acupuncture point GB37 (Guangming), located on the lower leg, is indicated for the treatment of vision related disorders within the TCM system. The name of the point, Guangming, is translated as bright light and indicates the acupoint’s use in the treatment of visual disorders. It is categorized as a Luo-connecting point and has the TCM functions of regulating the liver and clearing vision. The point is indicated for the treatment of hyperopia (farsightedness), myopia (nearsightedness), night blindness, and eye pain. The research demonstrates that GB37 increases neural responses in the occipital cortex. The researchers add that it was “discovered that modulations in vision-related cortex (BA18/19) were responsive to the specificity of GB37….” This connection between fMRI findings and TCM indications confirms the specificity of GB37 for the treatment of visual disorders.
Many examples of acupoint cortical specificity were included in the research. The following are some highlights. The researchers note, “Acupuncture at the three classical acupoints of Hegu (LI4), ST36 and Taichong (LV3) produced extensive deactivation of the limbic-paralimbic-neocortical brain network as well as activation of its anti-correlated activation network.” Differentiation between the points was noted as the following, “LI4 was predominant in the pregenual cingulated and hippocampal formation, ST36 response was predominant in the subgenual cingulate, and LV3 in the posterior hippocampus and posterior cingulated….” Taixi (KI3) mediated the executive network, Qiuxu (GB40) activated the auditory network, and “Jiaoxin (KI8) was associated with (the) insula and hippocampus in pain modulation.”
The mechanisms of cerebral action of true acupuncture were found distinct from sham acupuncture. The researchers note, “Acupuncture at Taichong (LR3) could specifically activate or deactivate brain areas related to vision, movement, sensation, emotion, and analgesia compared with sham acupuncture.” They add, “Several studies have found that there were different brain responses between traditional acupoints and sham points….” It was found that “ST36 could induce greater activation in ventrolateral periaqueductal gray (PAG) and produced linearly time-variant fMRI activities in limbic regions, such as amygdale and hippocampus….” Needling acupuncture point Erjian (LI2) activated the insula and operculi but this did not occur with sham acupuncture. Other research examples were cited. The researchers concluded, “These results provided evidence to support that acupoints may have its own functional specificity to sham point.”
Reference
He, Tian, Wen Zhu, Si-Qi Du, Jing-Wen Yang, Fang Li, Bo-Feng Yang, Guang-Xia Shi, and Cun-Zhi Liu. "Neural mechanisms of acupuncture as revealed by fMRI studies." Autonomic Neuroscience (2015).
Biochemical Changes and Acupuncture
Researchers have discovered that acupuncture causes a special biochemical reaction that reduces inflammation and muscle pain. The study, published in Molecular Neurobiology, investigated the effects of needling one acupuncture point on the leg. The research team measured a remarkable effect.
Manual acupuncture stimulation downregulated M1 macrophages (pro-inflammatory cells) and upregulated M2 macrophages (anti-inflammatory cells). As a result, acupuncture reduced pain and swelling. This neurobiological acupuncture continuing education study solves a great mystery, how does acupuncture work? The secret is in the biochemistry. M2 macrophages are an important source of IL-10 (interleukin-10), an anti-inflammatory cytokine that plays an important role in immune responses. Cytokines are proteins released by cells that regulate reactions between cells. Manual acupuncture successfully downregulates M1 macrophages and upregulates M2 macrophages thereby promoting the release of greater IL-10 concentrations. As a result of IL-10 release, pain and inflammation significantly reduce.
This study measured responses in muscle tissues and confirmed that M1 to M2 macrophage phenotype switching is triggered by acupuncture stimulation. Acupuncture literally flips a switch wherein initial inflammatory responses are reduced and the secondary healing responses are promoted. M1 macrophage downregulation and M2 macrophage upregulation triggered by acupuncture was positively associated with reductions in muscle pain and inflammation.
The researchers tested the biochemical process by adding an IL-10 blocking agent in the laboratory experiment. When IL-10 was chemically blocked, acupuncture did not reduce pain and swelling. However, when no blocking agent was applied, acupuncture successfully reduced both pain and swelling. The M2 macrophage upregulation by manual acupuncture successfully created a greater source of IL-10. The researchers note, “These findings provide new evidence that MA (manual acupuncture) produces a phenotypic switch in macrophages and increases IL-10 concentrations in muscle to reduce pain and inflammation.”
Macrophages are required by the body to resolve muscle injury. During injury, M1 macrophages are produced and release inflammatory biochemicals including pro-inflammatory cytokines. M2 macrophages have anti-inflammatory properties and promote the release of interleukin-10. An injury process features an initial inflammatory stage wherein M1 pro-inflammatory macrophages are upregulated. A secondary recovery phase wherein M2 anti-inflammatory macrophages are upregulated helps to promote healing and repair. Manual acupuncture successfully triggered the phenotype switch wherein the M1 macrophages were downregulated and M1 macrophages were upregulated thereby allowing increased IL-10, reductions in pain and decreased swelling.
References
da Silva, Morgana D., Franciane Bobinski, Karina L. Sato, Sandra J. Kolker, Kathleen A. Sluka, and Adair RS Santos. "IL-10 Cytokine Released from M2 Macrophages Is Crucial for Analgesic and Anti-inflammatory Effects of Acupuncture in a Model of Inflammatory Muscle Pain." Molecular Neurobiology (2014): 1-13.
Rafael Torres-Rosas, Ghassan Yehia, Geber Peña, Priya Mishra, Maria del Rocio Thompson-Bonilla, Mario Adán Moreno-Eutimio, Lourdes Andrea Arriaga-Pizano, Armando Isibasi, Luis Ulloa. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nature Medicine, 2014; DOI: 10.1038/nm.3479.
Wang, Ying, Rebekka Gehringer, Shaaban A. Mousa, Dagmar Hackel, Alexander Brack, and Heike L. Rittner. "CXCL10 Controls Inflammatory Pain via Opioid Peptide-Containing Macrophages in Electroacupuncture." PloS one 9, no. 4 (2014): e94696.


