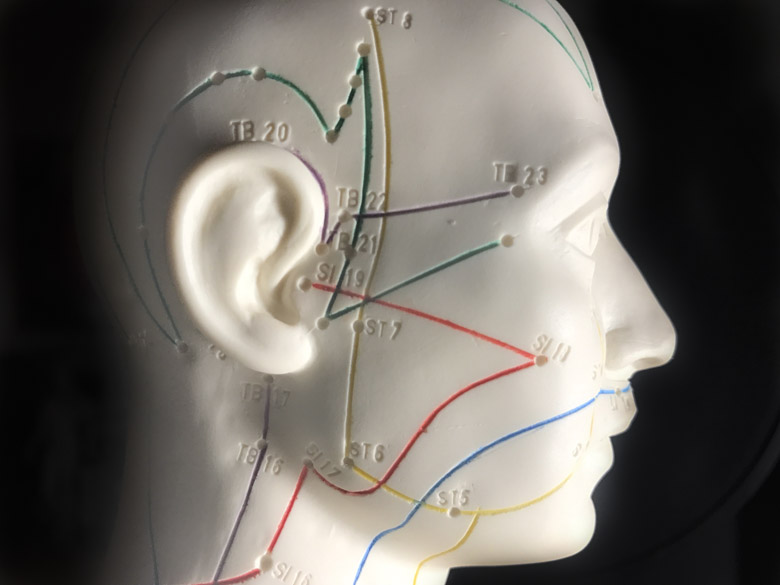
 Acupuncture points on the facePhotograph: © Healthcare Medicine Institute
Acupuncture points on the facePhotograph: © Healthcare Medicine Institute
Acupuncture relieves herpangina-related symptoms, speeds fever recovery time, accelerates the healing of herpangina sores, and reduces the recurrence of herpangina-induced fever. Herpangina is a viral pediatric illness that causes ulcers on the roof of the mouth and throat. There may also be comorbid fever, sore throat, headache, or neck pain.
Researchers at the Fifth People’s Hospital of Yuhang District, Hangzhou, combined acupuncture with standard drug therapy (ribavirin, an antiviral medication used to treat herpangina). Patients receiving both drug therapy and acupuncture in a combined treatment protocol had superior outcomes compared to patients using only acupuncture or only drug therapy.
Three groups were compared. The first group received both acupuncture and drug therapy. The second group received only acupuncture. The last group received only drug therapy. The acupuncture plus drug group had a 95.0% total treatment effectiveness rate, whereas the acupuncture group and the ribavirin medication group had 80.0% and 62.5% total treatment effectiveness rates, respectively.
In addition, fever recovery times, lesion healing times, and frequency of ibuprofen oral suspension tablets use consumed by all participants were also calculated. Compared with the acupuncture group and the ribavirin medication group, the acupuncture plus drug group had shorter fever recovery times and healing times. Moreover, the patients in the acupuncture plus drug group used less ibuprofen oral suspension tablets to reduce fever. There is a statistically significant difference between the acupuncture plus drug group and either of the two other groups. Based on the data, the researchers conclude that the combination of acupuncture and drug therapy produces superior positive patient outcomes for the treatment of infantile herpangina.
In Traditional Chinese Medicine (TCM), herpangina falls under the Hou Bi (translated as throat impediment) class of disorders. Herpangina treatment in TCM focuses on coursing wind and clearing heat. In the Chong Lou Yu Yao (translated as Jade Key to the Secluded Chamber), a TCM book of laryngology written in the Qing dynasty, it is said that “In throat inflammation, the zang organs such as the lung and stomach are contracted with wind evil. As a result, there might be deep-lying heat mixed with wind evil, leading to the blockage of qi and blood. Meanwhile, wind-phlegm may harass the upper body and produce toxic heat in the throat.” This book also mentions the treatment of herpangina. It is written that “For treatment, acupuncture should be used to free the meridians and activate qi and blood circulation. Once qi and blood circulation are free, wind-phlegm and toxic heat can be dissipated.”
Based on the above understanding of herpangina, the acupuncture protocol in this study involves the needling of Fengchi, Hegu, Quchi, Shaoshang, Shangyang, Xiaguan, Jiache, and Dicang. Hegu is a Yuan-Source point on the hand yangming large intestine meridian and indicated for fever and aversion to cold. Quchi is a He-Sea point on the hand yangming large intestine meridian and is indicated for fever and sore throat. Fengchi is a meeting point of the shaoyang meridians and the yangwei meridian. Needling this acupoint courses wind and resolves the exterior. Shaoshang is a Jing-Well point on the hand taiyin lung meridian. Shangyang is a Jing-Well point on the hand yangming large intestine meridian. These two acupoints are traditionally indicated for throat inflammation, and using the blood releasing technique on the acupoints clears lung-stomach heat. Jiache, Dicang, and Xiaguan are needled to activate qi and blood circulation in the yangming meridians, relieving herpangina-induced symptoms such as a loss of appetite and excessive saliva.
A total of 120 patients with infantile herpangina were treated and evaluated in this study. The patients were diagnosed with herpangina between July 2014 and October 2016. They were randomly divided into three groups: an acupuncture plus drug group, an acupuncture group, and a drug group, each consisting of 40 cases.
The statistical breakdown for each randomized group was as follows. The acupuncture plus drug group was comprised of 18 males and 22 females. The average age in the acupuncture plus drug group was 3 (±1) years. The average course of disease in the acupuncture plus herb group was 1.22 (±0.40) days. The acupuncture group was comprised of 21 males and 19 females. The average age in the acupuncture group was 3 (±1) years. The average course of disease in the acupuncture group was 1.20 (±0.41) days. The drug group was comprised of 19 males and 21 females. The average age in the drug group was 3 (±1) years. The average course of disease in the drug group was 1.25 (±0.44) days. There were no significant statistical differences in terms of age, gender, and course of disease relevant to patient outcome measures.
Inclusion criteria were as follows. According to the Science of Pediatrics (6th Edition, Chinese People’s Medical Publishing House), patients participating in the study met the following criteria:
- Between 1 – 7 years old
- Sudden high fever with sore throat, excessive saliva, loss of appetite, vomiting, and often throat congestion
- Dozens of 2 to 4 mm-diameter grayish vesicles with red surrounding irritations, which most often appear on the tonsillar pillars (adjacent to the tonsils), soft palate, or tonsils
Patients who had the following conditions were filtered out of the selection:
- Course of disease more than 2 days
- Absence of fever
- WBC (white blood cell) count more than 12×109/L
- Diagnosed with hand-foot-and-mouth disease
- Severe primary and concomitant cardiovascular, liver, kidney, digestive, or hematopoietic diseases
For the drug group patients, 10 mg/kg of ribavirin granules were prescribed for oral administration daily at a rate of three times per day for a total of 3 days. For the acupuncture group patients, these were the selected acupoints:
- GB20 (Fengchi)
- LI4 (Hegu)
- LI11 (Quchi)
- ST7 (Xiaguan)
- ST6 (Jiache)
- ST4 (Dicang)
- LU11 (Shaoshang)
- LI1 (Shangyang)
Treatment commenced with patients in a sitting position under the supervision of their parents. After disinfection of the acupoint sites, a 0.30 mm x 25 mm disposable filiform needle was inserted into each acupoint. For Fengchi, Hegu, Quchi, Xiaguan, Jiache, and Dicang, the needle was inserted at a high entry speed, reaching a depth of 8 mm. A one-minute needle retention time was observed. During the needle retention time, Fengchi, Hegu, and Quchi were applied with the Xie (attenuating) technique whereas Xiaguan, Jiache, and Dicang were applied with the Ping Bu Ping Xie (attenuating and tonifying) manipulation technique. Next, the needles were withdrawn slowly. For Shaoshang and Shangyang, the local skin was pricked and squeezed to obtain three drops of blood. The acupuncture session was conducted daily for 3 consecutive days.
During treatment for patients receiving drug therapy, the participants were asked to take ibuprofen orally when their body temperature was above 39°C. Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can be used to treat fever. The treatment effectiveness was evaluated using the herpangina symptoms and signs rating, and they were categorized as follows:
- Significantly effective: Rating reduction of at least 70%.
- Effective: Rating reduction of at least 30%.
- Ineffective: Rating reduction of less than 30%.
The three groups showed positive outcomes. However, the acupuncture plus drug group had a 95% effectiveness rate whereas the acupuncture group and the ribavirin medication group had 80% and 62.5% total effectiveness, respectively. Thus, there were statistically significant differences between the groups.
Reference:
Lang X, Wang YS, Wang XJ, Li JE, & Zhang YM. Clinical Observation of Infantile Herpetic Angina Treated with Acupuncture: A Randomized Controlled Trial [J]. Chinese Acupuncture and Moxibustion, 2017, (06):613-616.


