Researchers determined that a combination of acupuncture and McKenzie physical therapy produces excellent results for patients with cervical spondylosis, a painful disorder caused by intervertebral disc degeneration. Patients receiving only acupuncture had a 96.7% total effective rate and patients receiving McKenzie therapy had a 63.3% total effective rate. However, when the two therapies were combined into a comprehensive treatment protocol, the total effective rate was 100%.
Cervical spondylosis is a type of neck osteoarthritis involving the facet joints and intervertebral discs. Chronic improper biomechanical functioning of the cervical spine leads to degeneration of the neck’s bones and cartilage. Symptoms range from mild to severe and include pain of the neck and shoulders, stiff neck, muscle weakness, dizziness, and numbness. Southern Medical University, School of Traditional Chinese Medicine (Guangzhou, China) researchers investigated the analgesic effects of abdominal acupuncture combined with McKenzie therapy for patients with cervical spondylosis.
Classical Traditional Chinese Medicine (TCM) references do not specifically reference the term cervical spondylosis. As a result, cervical spondylosis is classified in several TCM categories Gu Bi, Yin Bi, Jing Jian Tong, Jian Bei Tong, Jing Jin Ji, Bi Zheng, Xiang Qiang (Zheng, Gang & Kong). Each of these categories includes specific instructions for identifying a clinical diagnosis and treatment regimen. For example, Gu Bi is translated as bone impediment. According to the Huangdi Neijing (Yellow Emperor’s Classic of Medicine), Gu Bi is caused by the congestion of wind, cold, and dampness. In addition, liver and kidney deficiency precipitates bone impediment. The treatment principle is to tonify the liver and kidneys, release the stagnation, and expel the exogenous pernicious influences.
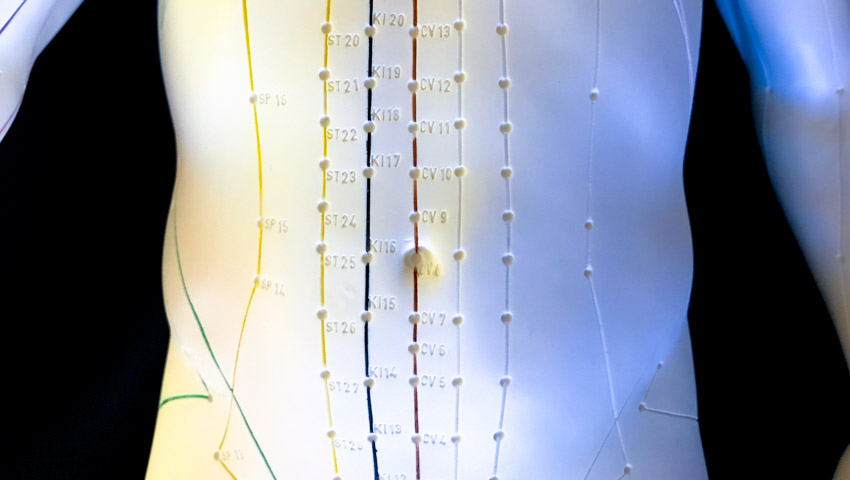
This clinical trial stands apart from many other investigations on the effects of acupuncture for the treatment of neck pain and dysfunction. Other investigations often include standard local and distal acupoints for the treatment of neck pain. In this investigation, abdominal acupuncture using Professor Bo Zhi Yun’s approach to patient care was implemented. This is a micro-needling system centered around acupuncture point Shenque (CV8). The central principle is to regulate the jing, qi, and blood to benefit internal organs and to promote healing. The following acupoints were needled:
- Zhongwan (CV12)
- Guanyuan (CV4)
- Shangqu (KD17)
- Huaroumen (ST24)
Patients rested in a supine position and all areas were disinfected prior to needle insertion. Single use, stainless steel, sterile filiform acupuncture needles (1.5”, 32 gauge) were used. Needling depth was approximately 1”, but varied according to patient size and point location in order to avoid the peritoneal cavity. Importantly, only licensed acupuncturists applied the needles to assure patient safety. Zhongwan was needled to promote the health of the spleen and stomach. Both Guanyuan and Zhongwan were needled more deeply than the other points.
Shangqu was needled to a shallow depth relative to the other acupoints. The point was used to promote blood circulation to the neck. This acupoint is traditionally needled to treat digestion disorders. It is the meeting point of the kidney channel with the penetrating vessel. This gives us insight into Professor Bo Zhi Yun’s use of this acupoint for cervical vertebrae disorders. The penetrating vessel has a branch that originates in the lower abdomen. In women, this branch originates in the uterus. The branch emerges at Huiyin (CV1) and then ascends inside the spinal column, from the sacrum to the cervical vertebrae. In this way, Shangqu connects to the cervical vertebrae through activation of the penetrating vessel.
Huaroumen was needled to a medium depth relative to the other acupoints. It was used to dredge the channels and promote qi circulation in the limbs and head. Other commentaries in the study note that needling Shangqu and Huaroumen quickly mitigates neck pain. Upon arrival of deqi at the acupoints, the rotating manual acupuncture technique was applied for one minute, once every five minutes. Each acupuncture session lasted a total of thirty minutes. Acupuncture was applied once per day, five times per week, for a total of ten times over a two week period.
Patients receiving only McKenzie therapy or McKensie physical therapy plus acupuncture had treatments once per weekday for two weeks. The researchers outline some of the basics of the physical therapy procedures used in the trial. McKenzie therapy began with patients seated in a chair with back support, in order to protrude the lumbar vertebrae forward. Next, five steps of physical therapy were administered. A hallmark of McKensie physical therapy treatment is self-care by patients. In the five steps, patients are empowered to learn exercises that they may ultimately practice independently.
- First, patients were asked to move their heads rearwards as much as possible and to stop movement for a short moment when their heads reached the maximum rearwards extent. Subsequently, patients moved their heads back to the original position. This process was repeated rhythmically. The patients were asked to try increasing the head rearward movement extent in each repetition.
- In step two, patients initiated rearward contraction and extension. The first part of this exercise is similar to step one. Next, with the head in the maximum rearward position, patients were asked to carefully and slowly extend their head and neck in all directions, and to stop movement for one second when their heads reached the final extension position. Next, the patients moved their heads back to the starting position.
- Step three involved rearward contraction and lateral bending. Based on rearward contraction procedures, the patients were asked to do head lateral bending, and stopped movement for one second when their head had reached the final bending position. Next, patients moved their heads back to the starting position.
- Step four involved rearward contraction and rotation. The patients began with rearward contraction. Subsequently, based on rearward contraction procedures, the patients were asked to rotate their head towards the affected side. The head remained contracted rearwards while rotating. Head movement was stopped for one second when their heads had reached the final rotation position, then the patients moved their head back to the starting position.
- In step 5, bending was used. The patients were asked to bend their heads downwards until the lower jaw reached the sternum, then the head moved back to its original position.
The above five steps were repeated rhythmically for a total of ten times per session. The entire process lasted 15–20 minutes per physical therapy session. McKenzie therapy was conducted once per weekday, for two weeks.
Acupuncture, as a standalone procedure, achieved a 96.7% total effective rate and McKenzie therapy, as a standalone procedure, achieved a 63.3% total effective rate. Combined, the therapies achieved a 100% total effective rate. The total effective rate ranged from patients having significant improvements to cured. The results indicate that a combined protocol of physical therapy and acupuncture, performed by a licensed acupuncturist, is an optimal treatment protocol for patients with cervical spondylosis.
References
Fu HL, Qu SS, Chen JQ, et al. (2013). Chinese Journal of Rehabilitation Medicine. 28(5): 418-422.
Zheng XF, Gang JP, Kong QX. (2005). Research on neck cervical spondylosis. Journal of Veterinary. 9(21): 672-673.


