Acupuncture is effective for the treatment of chronic fatigue syndrome (CFS). Researchers at the Beijing Chaoyang Fatou Community Health Service Center conducted a study comparing the effects of warm needling acupuncture, standard acupuncture, and sham acupuncture. [1] Based on the data, the researchers conclude that warm needling acupuncture is significantly more effective than using only standard acupuncture or sham acupuncture.
Three groups were compared. In one group, patients received sham acupuncture (a placebo control system used to simulate true acupuncture used in single-blinded and double-blinded trials). In the second group, patients received standard acupuncture as a means to control chronic fatigue syndrome. In the third group, standard acupuncture was combined with moxibustion therapy. The results demonstrate that sham acupuncture does not produce significant positive patient outcomes; however, standard acupuncture and warm needling acupuncture produce significant clinical results. The researchers note, “Acupuncture (and moxibustion) can be used as alternative and safe treatment protocols for chronic fatigue syndrome.”
About CFS
Chronic fatigue syndrome is defined as an illness characterized by severe disabling fatigue lasting for at least six months that is worsened by minimal physical or mental exertion. In the sphere of biomedicine, no definitive etiology has been identified. There are no key features or typical symptoms, but a sore throat, depression, and myalgia may all be present. [2]
The biomedical etiology of chronic fatigue syndrome (CFS) remains unclear. However, it has been suggested that psychological and social factors, viral loads, and immune system dysfunction may contribute to the condition. Previous studies find that CFS may be associated with a bias towards a Th2 type of response in Th1/Th2 immune balances. [3] Acupuncture’s ability to balance Th1 and Th2 may be one mechanism responsible for its effective action in the treatment of CFS.
Th1 (T helper 1) and Th2 (T helper 2) cells are types of T cells that play important roles in the adaptive immune system. Th1 cells secrete IL-2, interferon-gamma (IFN-γ), and tumor necrosis factor (TNF). Th2 cells produce IL-4, IL-5, IL-6, and IL-13. [4] In a Th2 immune response, IL-4 production by T cells is predominant over IFN-γ. Researchers Wang et al. note, “Acupuncturing at bilateral GV20 (Baihui), CV4 (Guanyuan), and ST36 (Zusanli) could elevate the serum IFN-γ concentration and the ratio of IFN-γ/IL-4 and regulate Th1/Th2 immune balance.” [5] This finding indicates that acupuncture may be of benefit to CFS patients with T cell imbalances.
Findings
The study involved 133 voluntary patients from the Beijing Chaoyang Fatou Community Health Service Center. All were diagnosed with CFS. Inclusion criteria were established based on the CDC (US Centers for Disease Control and Prevention) criteria for CFS and included the following:
- Experienced unexplained persistent or relapsing chronic fatigue for more than six months, which is not substantially alleviated by rest, and results in substantial reduction in previous levels of occupational, educational, social, or personal activities. [6]
In addition, the aforementioned is concurrent with four or more of the following symptoms:
- Substantial impairment in short-term memory or concentration
- Sore throat
- Tender lymph nodes
- Muscle pain
- Multi-joint pain without swelling or redness
- Headaches of a new type, pattern, or severity
- Unrefreshing sleep
- Post-exertional malaise lasting more than 24 hours
Acupuncture
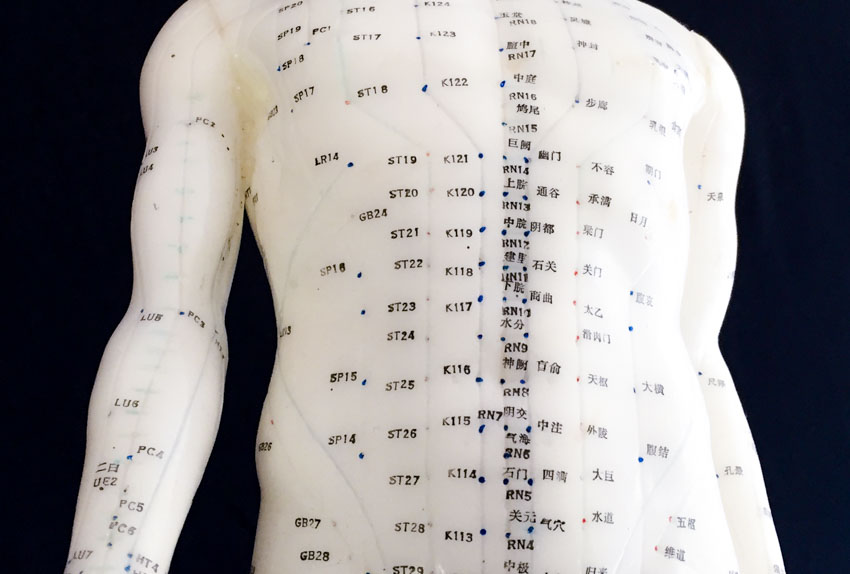
Patients were randomly divided into three groups: warm needling acupuncture group (n=44), acupuncture group (n=47), sham control group (n=42). For the warm needling acupuncture group, the average age of participants was 33.9 years. There were 20 males and 24 females. For the acupuncture group, the average age was 34.2 years (21 males and 26 females). For the sham control group, the average age of participants was 35.1 years (19 males and 23 females). The acupoints selected for the acupuncture and acupuncture plus moxibustion groups were the following:
- GV20 (Baihui)
- CV17 (Danzhong)
- CV6 (Qihai)
- CV4 (Guanyuan)
- ST36 (Zusanli)
- SP6 (Sanyinjiao)
- LI4, LV3 (Siguan: Hegu plus Taichong)
For the sham acupuncture control group, body points selected were neither meridian acupoints nor special acupoints. They were located at the following areas:
- 2 cm lateral to GV20
- 2 cm lateral to CV17
- 2 cm lateral to CV6
- 2 cm lateral to CV4
- 1.5 cm lateral to ST36
- 1.5 cm lateral to SP6
- 1 cm lateral to LI4, LV3
Chinese Medicine
The researchers provided a Chinese medicine theoretical basis for the protocols used in this acupuncture continuing education research. In Traditional Chinese Medicine, CFS falls in the scope of deficiency taxation (Xu Lao), wilting pattern (Wei Zheng), depression disease (Yu Bing), and hundred-union disease (Bai Hu Bing). CFS presentations are categorized into several differential diagnostic patterns including spleen qi deficiency, kidney jing-essence deficiency, spleen and kidney yang deficiency, liver depression, and qi stagnation. The treatment principle is to supplement deficiencies, support upright qi (Zheng Qi), and restore the liver’s function to control the smooth flow of qi.
Acupoints were selected to achieve the therapeutic actions guided by the treatment principles. Baihui is located on the Governing Vessel (Du Mai). Administering acupuncture at this acupoint lifts yang, boosts qi, and revives the spirit mind (shen). Danzhong, Qihai, and Guanyuan are located on the Conception Vessel (Ren Mai). Needling Danzhong restores the free flow of qi and supplements ancestral qi (Zong Qi). Acupuncture at the other two acupoints supports upright qi (Zheng Qi) and benefits the kidneys. Zusanli combined with Sanyinjiao is often used in modern clinical settings to strengthen the spleen and stomach and to benefit qi and blood. Siguan (a combination of bilateral Hegu and Taichong) was applied to restore the liver’s function to control the smooth flow of qi and activate qi and blood circulation.
For all three groups, each point was pierced with a disposable 0.25 mm × 40 mm needle (Huatuo brand), adhering to standard needling depths. For Baihui and Danzhong, the needles were inserted transverse-obliquely towards the direction of meridian energy flow. For the remaining acupoints, the needles were inserted perpendicularly. When a deqi sensation was obtained, Baihui, Qihai, Guanyuan, and Zusanli were manually stimulated with Bu (tonifying) manipulation techniques, while other acupoints were stimulated with the Ping Bu Ping Xie (attenuating and tonifying) manipulation techniques. Next, a needle retention time of 30 minutes was observed.
For the warm needling group, moxibustion was added to Baihui, Qihai, Guanyuan, and Zusanli. Medicinal moxa pieces of approximately 2 cm were attached to the needle handles and ignited. Thick paper heat shields were placed over the skin for protection. Moxa was left in place for 20 minutes per 30 minute needle retention time.
Acupuncture and moxibustion sessions were administered once per day. Each treatment course consisted of ten acupuncture treatments. All patients received two treatment courses in total. To evaluate the treatment effective rate, patients were scored before and after the treatments based on the Chalder Fatigue Scale as well as the Self-rating Satisfaction Scale. The Chalder Fatigue Scale is a measurement tool used for quantifying the severity of tiredness in CFS patients across multiple parameters (e.g., physical fatigue scores, mental fatigue scores, general fatigue scores).
After the treatment, the scores of the Chalder Fatigue Scale including physical fatigue scores, mental fatigue scores, and general fatigue scores were significantly decreased in the standard acupuncture and acupuncture warm needling groups, but not in the sham acupuncture group. The physical, mental, and general fatigue scores of the standard acupuncture and warm needling groups were significantly better than those of the sham acupuncture group, while the physical and general scores of the warm needling group were markedly better than those of the standard acupuncture group (P<0.05). Interestingly, the CFS patients’ satisfactory rates of the standard acupuncture and acupuncture plus warm needling groups were 36.2% (17/47) and 72.7% (32/44) respectively—indicating that moxibustion was well-received by patients. All groups had no adverse effects resulting from treatment or other medical procedures in the protocols.
The results indicate that warm needling acupuncture or standard acupuncture is more effective than sham acupuncture. The study by Lu et al., mentioned in this report, demonstrates that acupuncture is safe and effective for the treatment of chronic fatigue syndrome. Important features of TCM protocols are that they produce a high total effective rate without any significant adverse effects.
Summary
Major causes of suffering include pain, paralysis, mental illness, nausea, immune system imbalances, and fatigue. CFS and other clinical scenarios involving severe fatigue are a significant source of suffering and may be as severe as any other form of illness or complication. One concern is that since there is no clearly defined etiology within hospital medicine for CFS, patients may be marginalized or receive incomplete care.
There are instances in which patients are given psychiatric medications without addressing the biophysical sources of CFS. This focus on treating only the symptom and not the root cause of CFS potentially leads to prolonged suffering. Given the results of the research data, acupuncture with moxibustion is a reasonable treatment option, referable by primary healthcare physicians.
Notes
[1] Lu C, Yang XJ, Hu J. Randomized Controlled Clinical Trials of Acupuncture and Moxibustion Treatment of Chronic Fatigue Syndrome Patients. Acupuncture Research, 2014, 39(4):313-317.
[2] Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome. a comprehensive approach to its definition and study. Ann Intern Med. 1994;121:953 – 9. International Chronic Fatigue Syndrome Study Group.
[3] Skowera, A et al. “High Levels of Type 2 Cytokine-Producing Cells in Chronic Fatigue Syndrome.” Clinical and Experimental Immunology 135.2 (2004): 294–302.
[4] Choi, P, and H Reiser. “IL-4: Role in Disease and Regulation of Production.” Clinical and Experimental Immunology 113.3 (1998): 317–319.
[5] Wang XY, Liu CZ, Lei B. “Effect of Manual Acupuncture Stimulation of Baihui, Guanyuan, Zusanli on Serum IFN-γ and IL-4 Contents in Rats with Chronic Fatigue Syndrome.” Acupuncture Research 2014, 39 (05): 387 – 389.
[6] Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The Chronic Fatigue Syndrome: A Comprehensive Approach to its Definition and Study. Ann Intern Med. 1994 Dec 15;121(12):953-9.


