Acupuncture is effective for the alleviation of chronic obstructive pulmonary disease (COPD). First Affiliated Hospital of Guangzhou Medical University researchers compared the efficaciousness of true acupuncture and sham acupuncture. The combination of true acupuncture plus standard aerobic training produced superior patient outcomes over patients receiving sham acupuncture plus identical standard aerobic training. The researchers conclude, “the addition of acupuncture to a standard aerobic training regimen improves the exercise tolerance in COPD patients and strengthens the effectiveness of aerobic training.” In addition, they note that “acupuncture combined with aerobic training effectively improves the pulmonary function and quality of life.” [1]
Exercise tolerance, pulmonary ventilation function, and quality of life were measured before and after treatment. The 6-minute walking distance (6-MWD), exercise duration, and maximum oxygen uptake (VO2max) tests were recorded as indices of exercise tolerance. The 6-min walking test has been widely used to assess exercise tolerance in patients with chronic obstructive pulmonary disease (COPD). [2] Exercise duration refers to the length of time in which exercise is performed until an anaerobic threshold (AT) is reached. Maximum oxygen uptake (VO2max) is the gold standard for assessing aerobic capacity. [3]
Pulmonary ventilation function was evaluated based on percentages of predicted forced expiratory volume in 1 second values (FEV1%), percentages of predicted forced vital capacity value (FVC%), FEV1/FVC ratio, and percentages of predicted maximum ventilatory volume (MVV%). In addition, quality of life was documented using St. George's respiratory questionnaire (SGRQ). There was no statistically significant difference between the two groups’ baseline measurements (p>0.05) prior to treatments.
Exercise Tolerance
The true acupuncture group (standard acupuncture) significantly outperformed the sham acupuncture (control) group. The 6-MWD increased from 426.88 ±132.92 m to 491.01 ±146.22 m in the standard acupuncture group, and from 398.34 ±113.09 m to 410.60 ±125.6 m in the control group. Exercise duration increased from 337.00 ±187.93 m to 431.70 ±202.94 s in the standard acupuncture group, and from 318.71 ±88.10 s to 323.51 ±130.13 s in the control group. VO2 max increased from 17.97 ±6.62 mL/(min·kg) to 19.36 ±7.83 mL/(min·kg) in the standard acupuncture group, and from 398.34 ±113.09 mL/(min·kg) to 410.60 ±125.6 mL/(min·kg) in the control group. The standard acupuncture group produced superior outcomes for the improvement of the 6-MWD and exercise duration, and there is a statistically significant difference between the two groups (P<0.01).
Pulmonary Ventilation Function
FEV1% increased from 41.72 ±17.95 to 46.96 ±21.00 in the standard acupuncture group, and from 36.16 ±16.29 to 36.00 ±15.49 in the control group. FVC% increased from 67.09 ±22.23 to 71.86 ±24.34 in the standard acupuncture group, and from 68.51 ±13.45 to 69.29 ±15.51 in the control group. FEV1/FVC increased from 51.71 ±15.79 to 55.27 ±14.28 in the standard acupuncture group, and from 44.83 ±14.86 to 42.81 ±14.13 in the control group. MVV% increased from 41.81 ±15.36 to 52.28 ±22.60 in the standard acupuncture group, and from 34.09 ±13.04 and 36.16 ±12.13 in the control group. The standard acupuncture group had significantly greater improvements across the aforementioned parameters (P<0.05, P<0.01). In addition, standard acupuncture produced significant improvements in quality of life scores (SGRQ).
Design
The randomized controlled trial used the following study design. A total of 30 patients were recruited for the study and were randomly assigned to the sham acupuncture control group or the standard acupuncture group. All had a confirmed diagnosis of COPD. All were in a stable phase of COPD and the study limited the age range from 45–80.
The following exclusion criteria were applied:
- Mental and neurological disorders (e.g., Alzheimer's disease, Parkinson's disease)
- Severe and comorbid heart disease, hematologic malignancies, or physical disabilities
- Pregnant or lactating
- Unable to comply with medical instructions
The standard acupuncture group was comprised of 15 males and 1 female, with a mean age of 64 ±6 years and a mean body mass index (BMI) of 22.81 ±1.91. The sham acupuncture control group was comprised of 12 males and 2 females, with a mean age of 67 ±6 years and a mean body mass index (BMI) of 21.59 ±1.99. There was no statistically significant difference between the baseline characteristics of the two groups (p>0.05) prior to treatments in the investigation.
Aerobic Training
Both groups received standardized aerobic exercise training. The training methods were as follows:
- Training instrument: Exercise bicycles (MONARK, Sweden)
- Time: 40 minutes
- Intensity: 60–100% of the target heart rate (THR)
- Endpoint: >7 points based on the Subjective Exercise Intensity Scale, or >14 points based on the Rate of Perceived Exertion (RPE) Scale
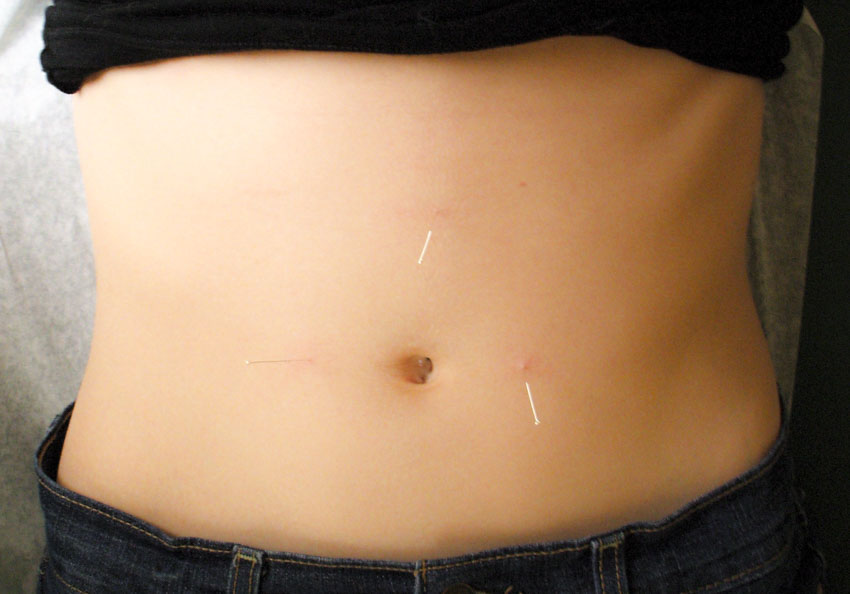
True and Sham Acupuncture
The primary acupuncture points used in the study included the following:
- CV17 (Danzhong)
- ST18 (Rugen)
- CV4 (Guanyuan)
- CV12 (Zhongwan)
- ST25 (Tianshu)
- ST16 (Yingchuang)
Secondary acupuncture points were added based on differential diagnostic pattern variations. For external pernicious influences, LI4 (Hegu) was added. For phlegm turbidity obstructing the center, ST40 (Fenglong) was added.
Standard acupuncture treatment was performed using filiform acupuncture needles. Electrical stimulation was also be applied to all acupoints at a low frequency (1–2 Hz), with a continuous wave, for 30 minutes. One acupuncture session was provided 2–3 times per week, for a total of five weeks.
Sham acupuncture treatment was performed using a needle-free guide tube by applying pressure to the acupoints without the use of a needle. Sham acupuncture was applied to the same acupuncture point areas as in the true standard acupuncture group. Next, an electrical stimulator was connected to the tubes, but without actual electrical stimulation.
Summary
The results of the investigation indicate that acupuncture integrative care provides significant benefits for COPD patients. These include improvements in exercise tolerance, pulmonary function, and quality of life scores. True acupuncture improvements were significantly greater than sham acupuncture changes. The findings indicate that acupuncture has the potential to improve clinical outcomes for COPD patients when combined with usual care. Patients interested in learning more about treatment are recommended to contact a local licensed acupuncturist.
References:
[1] Tong J, Guo YM, He Y, Li GY, Chen F, Yao H. Regulatory effects of acupuncture on exercise tolerance in patients with chronic obstructive pulmonary disease at stable phase: a randomized controlled trial [J]. Chinese Acupuncture and Moxibustion, 2014, 34(9):846-850.
[2] CarterR, Holoday DB. 6-minute walking for assessment of functional capacity in patients with COPD [J]. Chest, 2003, 123 (5): 1408-1415.
[3] American Thoracic Society, American College of Chest Physicians. ATS/ACCP statement on cardio-pulmonary exercise testing [J]. Am J Respir Crit Care Med, 2003, 167 (2): 211-277.


