Acupuncture demonstrates the ability to benefit patients with glaucoma. Modern research has determined that acupuncture benefits blood flow in the arteries of the brain and eyes. The results are confirmed with ocular blood flow (OBF) flowmeter readings for ocular pulse amplitude. Let’s take a look at the results, the acupuncture procedures that achieved the results, and a let’s start with a close look at glaucoma and the challenges it presents.
Primary open-angle glaucoma affects over 60 million people worldwide and is the most common cause of irreversible blindness. Although common treatments can help to delay the progression of the disease, glaucoma currently has no cure. However, ancient texts of Chinese Medicine, including Yin Hai Jing Wei (Essential Subtleties on the Silver Sea), a 15th century book on ophthalmology, have established treatment protocols for many eye diseases including glaucoma. To test ancient theory against a modern understanding of disease progression, there have been a number of studies published examining the use of Traditional Chinese Medicine (TCM), including herbs and acupuncture, for the treatment of glaucoma. Recently, researchers at the Department of Ophthalmology at the University Hospital (Dresden, Germany) investigated the short-term effects of acupuncture on different ocular blood flow parameters and found that acupuncture based on eye-specific protocols had reproducible and quantifiable effects on ocular blood flow in patients with primary open-angle glaucoma.
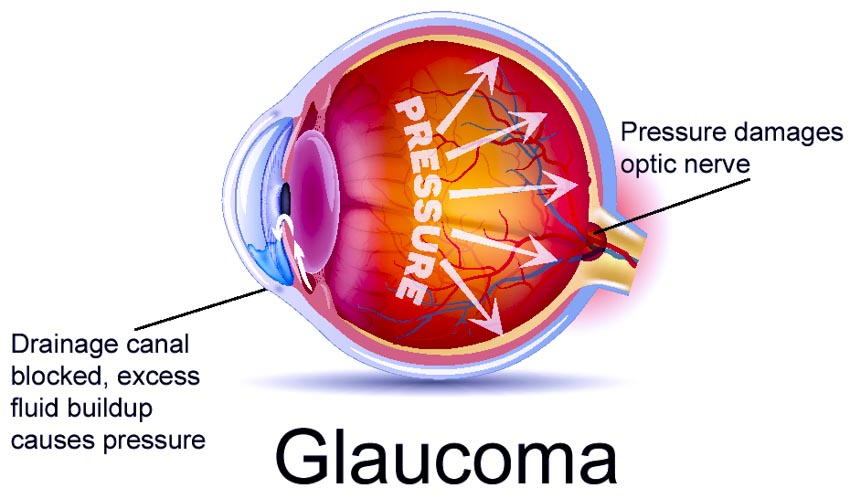
Glaucoma is defined by the “remodeling of the optic nerve head and a progressive loss of retinal nerve fibers” [1] beyond normal age-related decay; [2] this optic nerve degeneration eventually leads to visual field loss and, eventually, complete and irreversible blindness. [3] Of the 60 million people worldwide with glaucoma, between 4.5 and 8.4 million are blind as a result and, unlike blindness caused by cataracts (18 million worldwide), the progression of the disease cannot be reversed, which is why it is so important to manage the precipitating factors. [4]
Aqueous humor is a clear fluid continually produced by the eye. When the eyes are healthy, the amount of aqueous humor that is produced is equal to the amount that flows out of the eye. If the aqueous humor does not flow out of the eye properly, pressure in the eye builds up and causes ocular hypertension. [5] Intraocular pressure (IOP) is the most important factor in the progression of glaucoma; elevated IOP contributes to glaucomatous damage, and treatments that lower IOP are currently the standard of care for slowing nerve degeneration.
“Although IOP reduction is currently the main target for the treatment of glaucoma, treatment modalities that enhance retrobulbar hemodynamics in addition to reducing IOP may have a beneficial effect on the glaucoma therapy. It has been reported that glaucoma is associated with reduction in the blood flow velocity and elevation of the resistive index (RI) in the retrobulbar vessels. It has also been reported that patients with OAG [open angle glaucoma] have impaired hemodynamics in ophthalmic circulation.” [6] According to the vascular theory of glaucoma, optic neuropathy is a “consequence of insufficient blood supply due to either increased IOP or other risk factors reducing ocular blood flow (OBF).” [7] Others recently have begun to view glaucoma as a systemic disorder of the central nervous system (CNS).
Anatomically, the retina of the eye is part of the CNS: the axons of the retinal ganglion cells connect the eye directly to the brain through the optic nerve, which carries nerve impulses of visual input from the photosensitive rods and cones to the brain for processing. [8] “This anatomical continuity and the similarities at the molecular level are why glaucoma is increasingly considered together with other neurodegenerative conditions such as dementia,” [9] where apoptosis leads to neural degeneration. The consideration of glaucoma as a systemic disease has not yet led to any treatment strategies, but researchers are rethinking the possibilities and designing studies such as these which address other mechanisms of disease progression to test possible alternatives and complements to traditional care. “Sensory stimulation in the form of acupuncture/acupressure appears to have the potential to address all three areas of interest: IOP, blood flow and regulation of apoptosis.” [10]
The current standards of treatment revolve around lowering IOP. The first-line treatments for glaucoma are topical pharmacologic therapies: beta-blockers decrease aqueous humor formation and prostaglandin analogs increase the outflow of aqueous humor. [11] These topical agents are used initially “because they are effective, have relatively few ocular adverse effects, and can be used once or twice daily without affecting pupil size or accommodation,” two signs of neurologic health. [12] Second-line pharmacologic agents include alpha-agonists and topical anhydrase inhibitors decrease aqueous humor secretion, [13] but they may cause eye irritation and they must be used two or three times a day. [14] Parasympathomimetic (miotic) agents such as pilocarpine are used as third-line treatments because they affect pupil size or accommodation, and must be used two to four times daily. [15]
For those patients whose glaucoma cannot be controlled with medication, laser therapy and surgery are options. Laser trabeculoplasty increases drainage by promoting a biological and chemical change in the tissues and can be used in addition to, or instead of, medication, but it may in some cases cause an elevation of IOP. Incisional filtering surgery can also be used to create a new channel to improve the outflow of the aqueous humor. The most common surgery is trabeculectomy, in which “an opening created in the anterior chamber angle allows the aqueous humor to flow from the anterior chamber into a space beneath the conjunctiva under the surface of the eye,” [16] but there are a number of adverse effects associated with surgery. “The most common problem associated with this surgery is the growth of scar tissue, which may cause an obstruction in this artificial channel that blocks aqueous humor drainage, and the IOP-lowering effect may decrease gradually with time. Other vision-threatening complications include overfiltration, hypotony, bleeding, and infection.” [17] Non-penetrating surgical procedures have also been developed, such as viscocanalostomy and deep sclerectomy; these avoid full-thickness penetration of the anterior chamber of the eye and cause fewer adverse effects, but their efficacy is also compromised. [18] Despite the available treatments, glaucoma has no known cure, and some patients turn to traditional modalities to manage the condition. [19]
Acupuncture
Acupuncture has been used for centuries to treat ocular diseases, including glaucoma. Local points near the eyes, as well as distal points on related channels, have been the subject of modern research. “Accordingly to TCM, the zang gan (liver) and shen (kidneys) and their coupled fu dan (gall bladder) and Pangguang (bladder) have great influence in the preservation and energetic nutrition of the eye. Some previous studies suggested that local points act independently of the systemic acupuncture in some ocular dysfunctions.” [20] In 2011, Takayama et al. found that acupuncture therapy used in conjunction with standard medication “significantly decreased” [21] IOP, and cited another which demonstrated the capacity for acupuncture to improve choroidal blood flow in the eye. [22] “There are also studies of acupuncture treatments for primary open-angle glaucoma patients, including a recent study that examined the effect of acupuncture on intraocular pressure and ocular hemodynamics. This study had a small sample size (20 eyes) and no true placebo group, but it was able to show a decrease in IOP following acupuncture, and also reported Doppler imaging-based increases in ocular blood flow following treatment. The value of acupuncture, as with any other treatment approaches for the disease, will be measured in future studies that evaluate the ability of the technique to slow or reverse the retinal damage associated with POAG [primary open-angle glaucoma].” [23]
Some adverse effects have been reported with the use of some local points, especially those directly adjacent to the globe of the eye. In a case report published by Lee et al, the use of the points ST1 (Chenqi), and UB1 (Jingming) with strong needle stimulation caused traumatic optic neuropathy and globe perforation in one patient. [24] In this case, the practitioner mistook the patient’s complaints of pain for the de qi sensation mentioned in the ancient texts; “during the procedure, acupuncture needles are advanced deep into the acupoint to achieve an ache radiating to behind of the eye as describe in the Chinese literature.” [25] Because these points are anatomically sensitive, they must be needled with extreme caution, and with respect for patient feedback. While local points such as these may be anatomically predisposed to injury, local points slightly farther from the globe of the eye, such as UB2 (Zanzhu), Ex3 (Yuyao), SJ23 (Sizhukong), GB1 (Tongziliao), have also proved to be effective while offering less risk of injury. Additionally, in healthy controls, study outcomes have repeatedly shown that acupuncture has no effect on the IOP of patients with no ocular hypertension, [26] which matches the aim of acupuncture “to bring balance to the body energy.” [27]
Sensory Stimulation
Acupuncture, as a method for sensory stimulation, shows clinical potential for the treatment of glaucoma. In one report, it is noted, “Primary open-angle glaucoma is a group of optic neuropathies that can lead to irreversible blindness. Sensory stimulation in the form of acupuncture or ear acupressure may contribute to protecting patients from blindness when used as a complementary method to orthodox treatment in the form of drops, laser or surgery.” [28]
Sensory stimulation potentially has a profound impact on enhancing the pressure-lowering effect of standard treatments. Studies suggest it improves blood flow to the eye and optic nerve head, and “may play a role in neuroprotection through regulating nerve growth factor and brain-derived neurotrophic factor and their receptors, thereby encouraging the survival pathway in contrast to the pathway to apoptosis.” [29] Blood flow and neuroprotection are otherwise not directly influenced by standard treatment modalities. Acupuncture has also been associated with the release of certain neurotrophins, such as NGF [nerve growth factor] and BDNF [brain-derived neurotrophic factor], which have neuroprotective properties. [30] This increase in neurotrophins, along with an alteration of NGF receptors, is correlated with an increase in vascularization and a decrease in degenerate retinal architecture. [31] “There are now numerous suggestions that the potential neuroprotective effect of sensory stimulation may be achieved through reduction of the inflammatory drive and oxidative stress, regulation of neurotrophins, growth factors and, possibly uniquely, their receptors. All those markers of apoptosis are measurable, which will allow researchers in the future to determine the exact mechanisms responsible for apoptosis in cases of glaucoma.” [32]
Acupuncture Research
In this study, the researchers in Dresden, Germany investigated the effects of “eye-specific” acupuncture as compared to “eye-unspecific” acupuncture on different OBF parameters for patients treated with topical antiglaucoma medication. [33] For the eye-specific protocol, they used UB2 (Zanzhu), Ex3 (Yuyao), SJ23 (Sizhukong), GB1 (Tongziliao), SI6 (Yanglao), and GB37 (Guangming). For the eye-unspecific protocol, the points used instead were REN6 (Qihai), PC6 (Neiguan), ST36 (Zusanli), and SP6 (Sanyinjiao).
To measure blood flow, they used a number of different tests: the Heidelberg retina flowmeter (HRF) for parapapillary retinal blood flow, the OBF flowmeter for ocular pulse amplitude, pulsatile OBF, and IOP, and the dynamic vessel analyzing software (DVA), which allows the “precise determination of retinal vessel diameter with a time resolution of 25 readings/sec.” [34] The results of the HRF and DVA showed no significant changes after acupuncture with either point protocol. [35] However, measurements of OBF showed that eye-specific acupuncture “produces a specific reproducible and quantifiable effect on blood flow in the arteries of the brain and the eye,” [36] whereas the eye-unspecific acupuncture protocol did not have a statistically significant impact on retinal blood flow. More research is necessary to better understand the impact this may have on glaucoma treatment, but this suggests that acupuncture can have a multifactorial impact on thwarting the progression of glaucoma.
While standard usual care medicine can be effective lowering IOP in patients with glaucoma, there are as of yet no treatments that address the other risk factors, such as OBF and apoptosis, and a proportion of patients are still blinded by the disease every year. This new research has helped to show that “sensory stimulation may contribute to normalising IOP and blood flow to the eye and optic nerve as well as having a neuroprotective effect through both the regulation of neurotrophins and their receptors. Sensory stimulation may contribute to prevent progression of visual field defects and thereby delay blindness.” [37] Although the full picture is yet unclear, sensory stimulation, including acupuncture, should be seriously considered as an inexpensive and safe complement to standard procedures for the treatment of glaucoma.
References
[1] Anna Leszczynska et al., "The Short-term Effect of Acupuncture on Different Ocular Blood Flow Parameters in Patients with Primary Open-angle Glaucoma: A Randomized, Clinical Study," Clinical Ophthalmology Volume 12 (2018): pg 1285.
[2] Simon Law and Tianjing Li, "Acupuncture for Glaucoma," Cochrane Database of Systematic Reviews, 2006, pg 2.
[3] Edith Rom, "Sensory Stimulation for Lowering Intraocular Pressure, Improving Blood Flow to the Optic Nerve and Neuroprotection in Primary Open-angle Glaucoma," Acupuncture in Medicine 31, no. 4 (2013): pg 416.
[4] Rom, pg 416.
[5] aao.org/eye-health/diseases/ocular-hypertension-cause
[6] Shin Takayama et al., "Short-Term Effects of Acupuncture on Open-Angle Glaucoma in Retrobulbar Circulation: Additional Therapy to Standard Medication," Evidence-Based Complementary and Alternative Medicine 2011 (2011): pg 1.
[7] ncbi.nlm.nih.gov/pubmed/12150988
[8] ncbi.nlm.nih.gov/books/NBK10885/
[9] Rom, pg 416.
[10] Rom, pg 417.
[11] Law et al, pg 5.
[12] Law et al, pg 5.
[13] Law et al, pg 5.
[14] Law et al, pg 5.
[15] Law et al, pg 5.
[16] Law et al, pg 5.
[17] Law et al, pg 5.
[18] Law et al, pg 5.
[19] Law et al, pg 6.
[20] D. Meira-Freitas et al., "Short-term Effect of Acupuncture on Intraocular Pressure in Healthy Subjects," Acupuncture in Medicine 28, no. 1 (2010): pg 26.
[21] Takayama et al, pg 2.
[22] Takayama et al, pg 2.
[23] reviewofophthalmology.com/article/acupuncture-a-dry-eye-therapy-42260
[24] Wenyee Lee et al., "Traumatic Optic Neuropathy Secondary to Acupuncture Treatment for Glaucoma: A Case Report," Journal of Acute Disease 7, no. 3 (2018): pg 136.
[25] Lee et al, pg 136.
[26] Rom, pg 418.
[27] Meira-Freitas et al, pg 26.
[28] Rom, Edith. "Sensory stimulation for lowering intraocular pressure, improving blood flow to the optic nerve and neuroprotection in primary open-angle glaucoma." Acupuncture in Medicine 31, no. 4 (2013): 416-421.
[29] Rom, pg 416.
[30] Rom, pg 419.
[31] Rom, pg 419.
[32] Rom, pg 419.
[33] Leszczynska et al., pg 1286.
[34] Leszczynska et al., pg 1288.
[35] Leszczynska et al., pg 1288.
[36] Leszczynska et al., pg 1289.
[37] Rom, pg 421.
Bibliography
1. Leszczynska, Anna, Lisa Ramm, Eberhard Spoerl, Lutz E. Pillunat, and Naim Terai. "The Short-term Effect of Acupuncture on Different Ocular Blood Flow Parameters in Patients with Primary Open-angle Glaucoma: A Randomized, Clinical Study." Clinical Ophthalmology Volume 12 (2018): 1285-291. doi:10.2147/opth.s170396.
2. Law, Simon, and Tianjing Li. "Acupuncture for Glaucoma." Cochrane Database of Systematic Reviews, 2006, 1-27. doi:10.1002/14651858.cd006030.
3. Rom, Edith. "Sensory Stimulation for Lowering Intraocular Pressure, Improving Blood Flow to the Optic Nerve and Neuroprotection in Primary Open-angle Glaucoma." Acupuncture in Medicine 31, no. 4 (2013): 416-21. doi:10.1136/acupmed-2013-010403.
4. aao.org/eye-health/diseases/ocular-hypertension-cause
5. Takayama, Shin, Takashi Seki, Toru Nakazawa, Naoko Aizawa, Seri Takahashi, Masashi Watanabe, Masayuki Izumi, Soichiro Kaneko, Tetsuharu Kamiya, Ayane Matsuda, Akiko Kikuchi, Tomoyuki Yambe, Makoto Yoshizawa, Shin-Ichi Nitta, and Nobuo Yaegashi. "Short-Term Effects of Acupuncture on Open-Angle Glaucoma in Retrobulbar Circulation: Additional Therapy to Standard Medication." Evidence-Based Complementary and Alternative Medicine 2011 (2011): 1-6. doi:10.1155/2011/157090.
6. ncbi.nlm.nih.gov/pubmed/12150988
7. ncbi.nlm.nih.gov/books/NBK10885/
8. Meira-Freitas, D., A. J. Cariello, R. C. Vita, A. Tabosa, and L. A. S Melo. "Short-term Effect of Acupuncture on Intraocular Pressure in Healthy Subjects." Acupuncture in Medicine 28, no. 1 (2010): 25-27. doi:10.1136/aim.2009.001081.
9. reviewofophthalmology.com/article/acupuncture-a-dry-eye-therapy-42260
10. Lee, Wenyee, Weemin Teh, Norlinamohd Ramli, and Ahmadmt Saad. "Traumatic Optic Neuropathy Secondary to Acupuncture Treatment for Glaucoma: A Case Report." Journal of Acute Disease 7, no. 3 (2018): 134-135. doi:10.4103/2221-6189.236829.


