Hunan University of Traditional Chinese Medicine researchers find acupuncture effective for the treatment of insomnia. Their controlled laboratory investigation finds acupuncture effective for the regulation of sleep latency and duration. In addition, the researchers identified important biological responses elicited by acupuncture responsible for its effective actions.
In a quantification of acupuncture’s mechanisms, the research team of Wu et al. identified biochemical responses elicited by the application of three acupuncture point prescriptions. Baihui (GV20) plus Shenmen (HT7), Baihui plus Sanyinjiao (SP6), and Baihui plus a non-acupuncture point increased levels of 5-HT 1a receptor mRNA while decreasing levels of 5-HT 2a receptor mRNA in the hypothalamus of insomnia model rats. The researchers conclude, “Although all three acupuncture prescriptions produced positive outcomes, Baihui plus Shenmen produced the most significant results.”
This finding confirms the Traditional Chinese Medicine (TCM) indication that Shenmen is an effective acupuncture point, specifically for the treatment of insomnia. In many ways, this is a very unusual laboratory experiment. The methodology to determine sleep latency and duration varies greatly from standard human clinical trials. Nonetheless, the biomarkers measured in this experiment are consistent with the findings.
Previous studies have found that 5-hydroxytryptamine (5-HT) regulates the sleep-awakening cycle. It promotes awakening but also induces non-rapid eye movement sleep (NREM). In addition, 5-HT can work with norepinephrine (NE) to trigger rapid eye movements (REM). [2] The 5-HT 1a receptor is a subtype serotonin receptor. When binding, 5-HT regulates REM sleep and REM latency. The 5-HT 2a receptor is another subtype of serotonin receptor and can trigger wakefullness. [3]
Design
Sixty rats were randomly divided into 5 groups, including a control group, a model group, a Baihui plus Shenmen group, a Baihui plus Sanyinjiao group, and a Baihui plus non-acupuncture point group, with 12 rats in each group. Parachlorophenylalanine (PCPA) was injected intraperitoneally to establish rat models of insomnia. PCPA is a 5-HT synthesis inhibitor. It can decrease 5-HT levels in the central nervous system (CNS). [4] In a laboratory setting, PCPA is commonly used to make insomnia model rats. After 36 hours of establishing the model, the rats showed symptoms such as loss of circadian rhythms, constant activity during the day and night, hypersensitivity to external stimuli (r.g., light, sound), and irritability.
Treatment
The control group received no intervention. The model groups were immobilized on a rat plate in a supine position, once a day, 30 min per session, for 7 consecutive days. The acupoints selected bilaterally for the three acupuncture treatment groups were the following:
- Baihui plus Shenmen group: GV20 (Baihui), HT7 (Shenmen)
- Baihui plus Sanyinjiao group: GV20 (Baihui), SP6 (Sanyinjiao)
- Baihui plus Non-acupoint group: GV20 (Baihui), non-acupuncture point on the arm
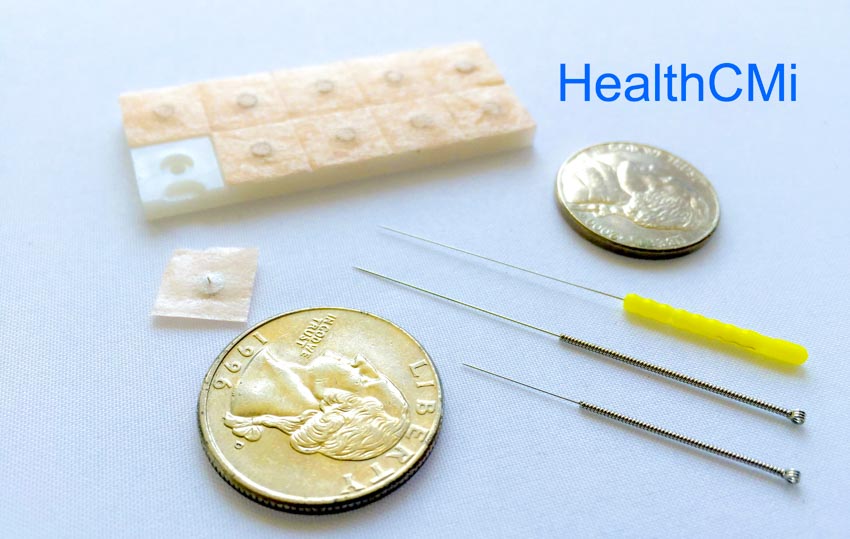
Upon disinfection of the acupoint sites, a 0.32 mm × 25 mm filiform acupuncture needle was inserted into the acupoints. For Baihui, the needle was inserted horizontally for 20 mm from back to front. For Shenmen, the needle was inserted perpendicularly, reaching a depth of 1 mm. For Sanyinjiao and the non-acupuncture point, the needle was inserted perpendicularly to a depth of 5 mm. The non-acupuncture point was located on the midpoint of the elbow tip and the armpit. After achieving a deqi sensation, the Ping Bu Ping Xie (attenuating and tonifying) manipulation technique was applied, with a twisting range of 180 degrees and a frequency of 60 times per minute. A 60 second manipulation was conducted every 10 minutes during each 30 minute needle retention time. The acupuncture treatment was conducted daily, for 7 consecutive days.
Results
Real-time fluorescence quantitative PCR was used to detect the expression of 5-HT 1a and 5-HT 2a receptor mRNA in the hypothalamus of the rats. The sleep latency and sleep duration were recorded. In this sodium barbital-induced sleeping study, sleep is defined as the time during which there is disappearance of righting reflex (self-correction of the body’s orientation). Awakening is defined as the time during which there is appearance of righting reflex. Sleep latency refers to the time between the injection of sodium barbital and disappearance of righting reflex. Sleep duration refers to the time between disappearance of righting reflex and awakening.
Compared with the control group, the expression of 5-HT 1a receptor mRNA in the model group was significantly decreased, and the expression of 5-HT2a receptor mRNA was significantly increased. Compared with the model group, the expression of 5-HT 1a receptor mRNA in the Baihui plus Shenmen group was significantly increased, and the expression of 5-HT2a receptor mRNA was significantly decreased. This is consistent with the testing of reflexes determining that this acupuncture combination benefits sleep.
Compared with the Baihui plus Shenmen group, the expression of 5-HT 1a receptor mRNA was significantly decreased in the Baihui plus Sanyinjiao group and the Baihui plus non-acupuncture point group. There was no significant difference in the expression of 5-HT 2a receptor mRNA between the Baihui plus Shenmen group and the Baihui plus Sanyinjiao group. The expression of 5-HT 2a receptor mRNA in the Baihui plus non-acupuncture point group was significantly higher. Compared with the control group, the model group had more delayed sleep latency. Compared with the model group, all three treatment groups had improved sleep latency.
Compared with the control group, the model group had shorter sleep duration. Compared with the model group, the Baihui plus Shenmen group had a longer sleep duration. There was no significant difference between the model group and the other two treatment groups. Among the treatment groups, the Baihui plus Shenmen group had longest sleep duration. There was no significant difference between the Baihui plus Sanyinjiao group and the Baihui plus non-acupuncture point group.
Summary
The results of the aforementioned research indicates that acupuncture is an effective treatment modality for the treatment of insomnia. Researchers demonstrate that acupuncture improves sleep latency and duration while simultaneously regulating pathways responsible for providing anti-insomnia effects to the hypothalamus of insomnia model rats.
Human clinical trials confirm that acupuncture is an effective modality for the treatment of insomnia. For example, China PLA Navy General Hospital researchers confirm that foot acupuncture alleviates insomnia. [5] Taipei Medical University researchers conducted a human clinical trial and determined that acupuncture regulates hormone levels and alleviates insomnia related to menopause. [6] In another human clinical trial, researchers find acupuncture more effective than estazolam (a benzodiazepine) for the treatment of insomnia. [7]
The aforementioned human clinical trials and others are included in the Healthcare Medicine Institute (HealthCMi) acupuncture continuing education course entitled Acupuncture For Insomnia. The online course covers diagnostics, acupuncture point prescriptions, and an array of scientific research demonstrating optimal acupuncture points for the treatment of sleep disorders. To see a sample of the course materials, click the following:
References
[1] Wu XF, Yuan JL, Zheng XN, Guo X, Chen XL, et al. Effect of Acupuncture Treatment on 5-HT1a and 5-HT2a mRNA Expression in Hypothalamus of Insomnia Rats [J]. Chinese Journal of Rehabilitation, ,2018, 33(05):360-364.
[2] Gu SZ, Dou DB. Research Progress of Traditional Chinese Medicine on HPA Axis Related Monoamine Neurotransmitters and Hormones in PCPA Insomnia Rat Model [J]. Journal of Shanghai University of Traditional Chinese Medicine, 2015, 29(1): 83-86.
[3] Sue JW, Jayne EB, Ann SR, et al. The use of sleep measures to compare a new 5HT1A agonist with buspirone in humans [J]. Nutt J Psychopharmacol, 2005, 19(11): 609-611.
[4] Gao HL, Tu X, Lu Y, et al. Rat model of Insomnia Caused by Heart and Kidney Disharmony [J]. Chinese Medicine, 2014, 36(6): 1138-1141
[5] Ma GH, Wei T & Chen TT. (2013). Efficacy of Treating Diseases by Managing Lower Plantar Acupuncture based Therapy in 42 Cases of Insomnia. JACM. 29(8).
[6] Hsiao-Yean Chiu, Yu-Jung Hsieh, and Pei-Shan Tsai, “Acupuncture to Reduce Sleep Disturbances in Perimenopausal and Postmenopausal Women,” Obstetrics & Gynecology 127, no. 3 (March 2016), pg 513.
[7] Wang YJ, Zhang LH, Han YX, Li PP. Efficacy observation on Governor Vessel-unblocking and mind-calming acupuncture for insomnia. Journal of Acupuncture and Tuina Science. 2016 Jul 1;14(4):274-8.


